Infant Botulism: Symptoms, Diagnosis, Treatment & Prevention
Proper care and hygiene in the initial weeks are essential for infant botulism recovery.

Image: ShutterStock
The absorption of toxins generated by the Clostridium botulinum bacterium, a rod-shaped spore-forming bacterium, causes infant botulism, a rare and possibly fatal illness. This bacterium thrives in the intestines and produces an enteric toxin that can cause intestinal immobility and paralysis.
Botulinum toxin is typically found on carpets and floors, and it can occasionally contaminate honey and grape molasses (1). The lack of protective intestinal flora and Clostridium-inhibiting bile acids in a baby’s intestines allows C. botulinum to flourish and colonize the large intestine, resulting in infant botulism.
While this bacterial infection primarily affects newborns aged one to six months, it has also been observed in babies as young as one week and as old as 12 months (2)
Read on to know the causes and symptoms of Botulinum infection in babies, how it can be detected early, and the available treatment options.
Signs and Symptoms Of Infant Botulism
Some of the symptoms of infant botulism include:
- Slowing down of breathing
- Drooping eyelids
- Floppy infant syndrome (low muscle tone)
- Poor feeding and weak sucking
- Loss of head control
- Lethargy
- Constipation
- Weak cry
- Muscle weakness
- Reduced gaging
- Paralysis that might spread downward (3)
The time from the appearance of early symptoms to the onset of severe complications ranges from less than 24 hours to more than a week. It is important to identify the signs of botulism early on to prevent complications. Next, let’s discuss the diagnosis of infant botulism.
Diagnosis
If your baby shows signs of respiratory distress or has difficulty breathing, it is best to take them to a pediatrician. Also, if the baby shows signs of relapse after getting discharged from the hospital, it is best to consult your doctor.
Botulism in babies can be identified through clinical tests, spinal fluid analysis, and electrodiagnostic testing imaging (EMG). The doctor might isolate the causative organism from the fecal matter to support the diagnosis. EMG is highly reliable for the diagnosis of infant botulism but might have false-positive results in some cases (2).
Risks And Complications Of Infant Botulism
According to a case-controlled study, decreased frequency of bowel movements, such as less than one per day for at least two months, is found to be the risk factor for botulism among infants who are older or less than two months. Breastfeeding and ingestion of corn syrup are also associated with the disease.
In infants younger than two months, living in the rural farming area was the only significant risk factor as per the same study (4).
If the disease is left unrecognized, it can lead to paralysis of the respiratory muscles, leading to low oxygen levels in the blood and respiratory arrest (5).
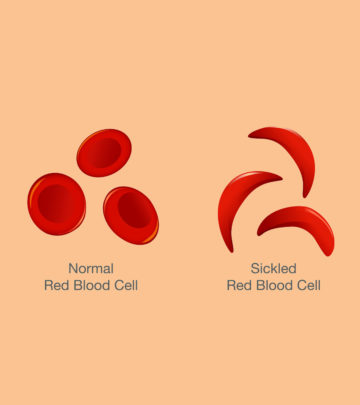
Other complications such as colitis, anemia, inappropriate antidiuretic hormone secretion, urinary tract infection, and secondary bacterial infections are also seen (6). Talk to your pediatrician if you have any questions.
Treatment For Infant Botulism
The disease’s natural course consists of a progression of weakness over one to two weeks until it worsens. If the baby is supported during this stage to avoid respiratory failure and flaccid paralysis, they may recover from the weakened state in two to three weeks without the requirement for botulism immune globulin intravenous (BIG-IV) (6).
BIG-IV works by neutralizing the free botulinum toxin. It may not show immediate improvement in the symptoms but help prevent the toxin from binding, thus helping in faster recovery. Studies state that babies who were given BIG-IV had a hospital stay for 2.6 weeks, while others stayed for 5.7 weeks (7).
Relapse of infant botulism may occur within 13 days of hospital discharge, so close monitoring is necessary during the first month after recovery (5).
Since bacteria cause the disease, care should be taken to prevent the infection spread. The patient’s excreta would contain the bacterial spores for weeks to months after the infection, so dispose of the stools appropriately, and wear gloves to prevent wound botulism (6).
Prevention Of Infant Botulism
Since the infection is spread through bacteria, you can prevent infant botulism by preventing the causative organism. Ensure to keep the premises clean and dustproof, and avoid feeding honey or products that may contain honey to babies under 12 months(4).
Frequently Asked Questions
1. How common is botulism in infants?
Out of 110 cases of botulism reported in the US annually, around seventy percent of these cases are infant botulism (8).
2. Can babies get botulism from honey nut cheerios?
Yes, babies under age one should not be given honey nut cheerios (9).
3. Can babies get botulism from breastmilk?
Since there is not enough medical evidence available on whether or not babies can get botulism from breastmilk, it is recommended that mothers suspected of botulinum poisoning should not breastfeed their babies (10).
Infant botulism is a rare but serious gastrointestinal condition caused by exposure to Clostridium botulinum (C. botulinum) spores. Bacteria from the spores can grow and multiply in a baby’s intestines, producing a dangerous toxin. The condition can occur in infants up to the age of 12 months. However, early identification of symptoms and medical support to prevent respiratory failure and flaccid paralysis can improve prognosis. If the disease is left unrecognized, it can lead to paralysis of the respiratory muscles, leading to low oxygen levels in the blood and respiratory arrest. So, to protect your baby from infant botulism, try to avoid exposure to potentially contaminated soil or dust.
Key Pointers
- Botulism usually affects babies aged one to six months as the gut microbiota, and bile acids are not well developed in an infant.
- Low muscle tone, lethargy, and slow breathing are symptoms seen in infants affected by this condition.
- Early identification of symptoms and medical support to prevent respiratory failure and flaccid paralysis can improve prognosis.
References
2. Eren Cagan, et al.; Infant Botulism; The Eurasian Journal Of Medicine (2010)
3. Infant botulism; MedlinePlus
4. JS Spika, et al.; Risk factors for infant botulism in the United States; American Journal of Diseases of Children (1989).
5. Nadine Cox and Randy Hinkle; Infant Botulism; American Family Physician (2002).
6. Emma McCutcheon, et al.; Infantile Botulism In British Columbia: A Case Report; British Columbia Medical Journal (2019).
7. Laura Jackson, et al.; Infant Botulism in the Very Young Neonate: A Case Series; AJP Reports (2017).
8. Botulism: Epidemiological Overview for Clinicians; The Centers for Disease Control and Prevention
9. Infant Feeding: 10-12 months; Child Health Specialty Clinics
10. Botulinum Poisoning; National Library of Medicine
Read full bio of Dr. Nikolina Zdraveska