Celiac Disease In Babies: 12 Key Symptoms To Watch For
Gastrointestinal issues such as vomiting may be symptoms; seek medical guidance for relief.
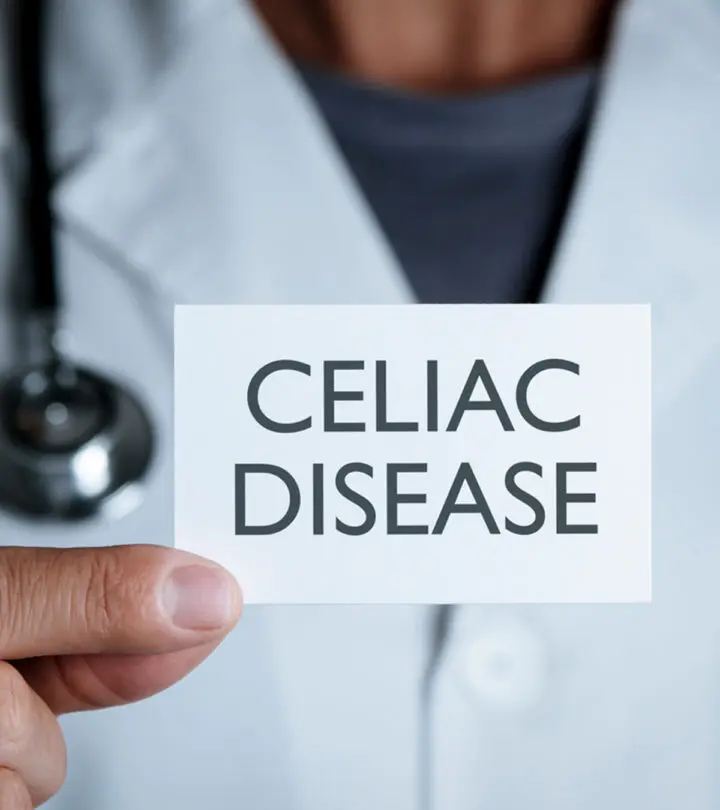
Image: iStock
If your infant is on formula or is ready to transition to solids, knowing about celiac disease in infants can help make informed choices. Celiac disease is an autoimmune disorder where gluten consumption, a protein found in wheat, barley, and rye, triggers autoimmune reactions in the body.
In this reaction, the body treats gluten as an antigen and attacks the small intestine, damaging its internal lining. This reaction results in the emergence of gastrointestinal signs and symptoms, which also help diagnose the condition. Treatment for the condition mainly involves eliminating gluten from the baby’s diet.
Keep reading to know more about the causes, symptoms, diagnosis, and treatment for celiac disease in babies.
What Causes Celiac Disease In Babies?
Celiac or Coeliac disease occurs when the body’s immune system abnormally recognizes gluten as a pathogen (1). Gluten is a protein found in wheat, rye, and barley. It is a protein also found in food items prepared from these grains. Grains that naturally do not contain gluten, such as oats and millets, could be contaminated with gluten if processed at the same facility that processes wheat, rye, and barley.
The abnormal immune response occurs due to atypical genetic mutations in the group of genes called the human leukocyte antigen (HLA) complex (2). These genes help the immune system cells distinguish the body’s proteins from other proteins, such as those found in pathogens.
Abnormal HLA genes make the immune system cells sensitive to a segment of gluten called gliadin. When the cells detect gliadin in the small intestine, they consider it to be a pathogen. The immune system triggers an immune response similar to the one seen in pathogenic cases. It results in inflammation, damaging the inner lining of the small intestine and causing celiac disease.
Risk Factors For Celiac Disease In Babies
Since genes govern abnormal immune responses in celiac disease, family history is usually considered to be the leading risk factor. Babies with parents or first-degree relatives with celiac disease may have a higher risk of developing the condition.
Infants and toddlers with the following conditions or disorders may also have a higher risk of developing celiac disease (3).
- Type 1 diabetes
- Selective immunoglobulin A deficiency
- Autoimmune thyroiditis
- Turner syndrome
- Down syndrome
- Williams syndrome
Not all babies with abnormal genes or risk factors may develop celiac disease. It is not known why some babies develop the condition. Environmental factors and the expressions of other genes may play a role in such cases (2).
Signs And Symptoms Of Celiac Disease
Most babies display gastrointestinal symptoms. These may vary depending on the intensity of their immune response and the quantity of gluten consumed (4) (5) .
- Abdominal bloating
- Vomiting
- Foul-odored diarrhea
- Fussiness and irritability
The repeated immune response to the gluten damages the villi found along the small intestine’s inner lining. The villi are finger-like projections that absorb nutrients from food. The immune response to gluten erodes and flattens the villi, making it difficult for the small intestine to absorb nutrients. It may gradually lead to the following symptoms.
- Malnutrition
- Iron deficiency anemia
- Low bone density
- Poor growth and short stature
- Chronic fatigue
- Poor weight gain or chronic weight loss
- Developmental delay
- Neurological problems
How Is Celiac Disease Diagnosed?
The diagnosis of celiac disease in babies is a multi-step procedure due to the similarities of its symptoms with those of other gastrointestinal conditions. The pediatrician will assess the symptoms and perform various tests to diagnose celiac disease (6).
Parents could be asked for details of the baby’s medical history, diet, and the duration of the symptoms. The following tests could be suggested to check specifically for celiac disease (7) (8).
- Blood test: Two to three milliliters of blood is drawn, usually from the baby’s heel. A tTG test is performed to assess the presence of anti-tissue transglutaminase antibodies, which are a type of IgA antibody. Individuals with celiac disease have a high number of these antibodies in their bodies.
- HLA test: It is a test that checks for the presence of human leukocyte antigen (HLA). Individuals with celiac disease have specific types of HLA. The presence of these HLAs may not confirm celiac disease but could indicate that the person is at a higher risk of developing celiac disease (9). This could help the doctor plan further testing or diagnostic procedures.
- Endoscopy with biopsy: An endoscopy is suggested if the tTG and HLA tests suggest the possibility of celiac disease. The baby is sedated with anesthesia, and an endoscopic tube is used to visualize the small intestine walls. The endoscope would contain tools to collect a small sample of the intestinal tissue for biopsy.
The doctor will review the blood tests, tests for other autoimmune diseases, the images of the intestinal walls, and the biopsy results to conclude the presence of celiac disease. It is essential you do not start a gluten-free diet for your baby before diagnosis since it may cause false-negative test results..
Treatment For Celiac Disease In Babies
There is no cure for celiac disease. The only way to avoid symptoms and discomfort is to stick to a gluten-free diet forever. Below are some salient attributes of the management of celiac disease in babies (10).
- You will need to eliminate all types or varieties of wheat, rye, and barley from the baby’s diet. The baby cannot have products, such as cakes, biscuits, and pies, made from these grains.
- In rare cases, gluten could be found in several medicines, processed foods, candies, toothpastes, skin products, and even paints found on some toys. Several celiac disease support organizations provide guidebooks about products that may potentially contain gluten.
- The baby may have gluten-free grains, such as millets and rice. The baby could also have pseudograins, such as quinoa and buckwheat. Soy, tapioca, and corn flours could make appropriate alternatives, too.
- Gluten-free grains could be contaminated with gluten if processed at the same facility where wheat, rye, or barley is processed. Check for the words “gluten-free” on the packaging. You may also check for gluten-free products specially made for those with celiac disease.
- Your baby’s pediatrician may refer you to a dietician who can plan an appropriate gluten-free diet plan for your baby. A dietician may also guide you on ways to avoid gluten in the baby’s diet.
Babies and toddlers could find relief from symptoms once gluten is eliminated from the diet. Since the baby can eat other food items, nutritional deficiencies seldom occur. Non-responsive celiac disease is considered when the baby shows no improvement. However, it occurs when the baby has other gastrointestinal conditions, such as lactose intolerance,or receives a small amount of gluten from some source (11).
In rare cases, some individuals may have refractory celiac disease (RCD), which does not respond to a gluten-free diet even after a year. RCD is extremely rare in children (12) (13).
Can Celiac Disease In Babies Be Prevented?
There is no definitive way to prevent celiac disease. A few studies suggest that babies be introduced to gluten-containing food items after six months of age while continuing breastfeeding. The research theorizes that the antibodies found in breast milk could help modulate a baby’s immune response, preventing abnormal reactions towards gluten (14). However, celiac disease tends to be genetic, and even those with genetic predisposition do not necessarily develop the disease. Therefore, there is no conclusive method to prevent the autoimmune disorder (15). Nevertheless, there are benefits of breastfeeding, including immunological benefits for the baby. You may ensure you continue to breastfeed your baby while introducing solids for at least six months of a baby’s age.
Frequently Asked Questions
1. Can breastfed babies have celiac disease?
Until the baby is only being breastfed, they can’t have celiac disease. However, once they begin consuming solid foods, they may develop celiac disease if they are sensitive to gluten. According to a study, the gradual introduction of gluten-containing foods in an infant’s diet who is still being breastfed reduced their risk of developing celiac disease in early childhood (16).
2. Can babies outgrow celiac disease?
Celiac disease is a chronic autoimmune condition that can’t be outgrown. However, one can manage the condition well with proper dietary alterations (8).
3. At what age is celiac disease diagnosed?
Many children are diagnosed with celiac disease between six months and two years of age (17). The diagnosis time coincides with the time when most children begin consuming gluten-containing solids.
Since celiac disease is an autoimmune condition, it is mostly genetically acquired and may run in families. Celiac disease in infants is characterized by gastrointestinal symptoms. Since babies with celiac disease have issues with nutrient absorption from the ingested food, you and the child’s healthcare provider need to keep an eye out for symptoms that may indicate malnourishment, anemia, low bone density, etc. While there is no cure for the disease, dietary modifications can help the baby lead a normal and healthy life.
Infographic: Common Misconceptions About Celiac Disease
Misconceptions are often common about chronic conditions that can be managed with dietary or lifestyle modifications. Celiac disease is no different. It is essential to know the facts about the diseases to follow an adequate diet and understand the outcomes. Go through the infographic to know some common misconceptions about celiac disease and the facts to debunk them.
![myths and facts about celiac disease [infographic]](https://cdn2.thebridalbox.com/wp-content/uploads/2021/07/Myths_And_Facts_About_Celiac_Disease-jpeg-scaled.jpg.webp)
Key Pointers
- Celiac disease in babies is caused by an abnormal immune response to the gluten protein.
- Vomiting or diarrhea, accompanied by bloating and crankiness are some symptoms.
- Blood test, HLA test, and endoscopy with biopsy help diagnose celiac disease.
References
- Celiac disease; Harvard Medical School
https://www.health.harvard.edu/diseases-and-conditions/celiac-disease - Celiac disease U.S. National Library of Medicine
https://medlineplus.gov/genetics/condition/celiac-disease/ - Anthony Porto Celiac Disease in Children & Teens; American Academy of Pediatrics
https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Celiac-Disease.aspx - Coeliac disease and breastfeeding; Australian Breastfeeding Association
https://www.breastfeeding.asn.au/bfinfo/coeliac-disease-and-breastfeeding - Celiac Disease in Children; Celiac Disease Foundation
https://celiac.org/about-celiac-disease/celiac-disease-in-children/ - Diagnosis of Celiac Disease; National Institutes of Health
https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease/diagnosis - How are infants tested for celiac disease?; University of Chicago Medicine
https://www.cureceliacdisease.org/faq/how-are-infants-tested-for-celiac-disease/ - Celiac Disease: Diagnosis & Treatments; Boston Children’s Hospital
https://www.childrenshospital.org/conditions-and-treatments/conditions/c/celiac-disease/diagnosis-and-treatment - Celiac Disease – Testing; Celiac Disease Foundation
https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/ - Treatment for Celiac Disease; National Institutes of Health
https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease/treatment - Non-Responsive and Refractory Celiac Disease; Beyond Celiac
https://www.beyondceliac.org/celiac-disease/refractory-nonresponsive-celiac-disease/ - Francesco Valitutti et al. Pediatric Celiac Disease; Pediatric Celiac Disease; Advances in Nutrition
https://academic.oup.com/advances/article/8/2/356/4558047 - Refractory Celiac Disease; National Organization for Rare Disorders
https://rarediseases.org/rare-diseases/refractory-celiac-disease/ - L.M. Sollid Breast milk against coeliac disease; U.S. National Library of Medicine
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1773451/ - Caroline Meijer et al. Celiac Disease Prevention; U.S. National Library of Medicine
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6284033/ - Anneli Ivarsson et al.; (2002); Breast-feeding protects against celiac disease.
https://pubmed.ncbi.nlm.nih.gov/11976167/ - Celiac Disease.
https://kidshealth.org/en/kids/celiac.html
Read full bio of Dr. Supriya Mahajan
Read full bio of Rohit Garoo