5 Signs, Symptoms & Treatment For Epilepsy In Children
Changes in behavior and abnormal movements are common signs of epilepsy.
Image: Shutterstock
In This Article
Epilepsy in children is a chronic non-communicable disease affecting the brain. The International League Against Epilepsy (ILAE) Task Force defines epilepsy as any of the below conditions (1):
at least two unprovoked seizures occurring more than 24 hours apart from one unprovoked seizure with a risk of recurrence in the next ten years an epilepsy syndrome.
The incidence rate of epilepsy is about 102/100,000 in children up to 12 years and 21–24/100,000 among children aged 11–17 years (1). Although the maximum incidence rate of epilepsy maps prevails during the first year of life, the symptoms of epilepsy may begin at any point of life, depending on its type.
Read about the causes, types, symptoms, risk factors, treatment, and prevention of epilepsy in children.
Causes Of Epilepsy In Children
The causes may vary depending on the type of epilepsy. However, some cases can be idiopathic (have unknown causes). Most children with epilepsy have one or more of the following conditions (2):
- Genetic changes that may or may not be inherited from one or both parents.
- Structural or symptomatic brain damage, such as a brain injury, brain infection, including meningitis, brain tumor, stroke, or brain development issues, can cause epilepsy in some children.
- Genetic conditions, such as neurofibromatosis or tuberous sclerosis, can cause structural brain changes, including brain growth, and trigger epilepsies.
Some researchers believe that the cause of epilepsy is genetic in most cases since seizure threshold (level of resistance to seizures) is a part of genetic makeup and varies in each child. Thus, the tendency of developing seizures after structural changes or brain injury may depend on genetic factors. This theory is justified since many children experience brain changes but not all develop seizures or epilepsy.
Risk Factors For Epilepsy In Children
The common risk factors for developing epilepsy in children may include (1):
- High temperature (fever)
- Mental disability
- Positive family history
- Alcohol use or smoking during pregnancy
- Delayed NICU discharge
- Premature birth
The probability of recurrent epilepsy is 30% in children with one seizure episode. However, the chance of recurrence can increase to more than 70% in children with all risk factors. In comparison, children with no risk factors have less than a 20% chance of recurrent episodes (1).
Signs And Symptoms Of Epilepsy In Children
Children with epilepsy can have seizures due to abnormal electrical activity in the brain. The symptoms of epilepsy may depend on the affected brain area. However, the following abnormalities are often seen in epilepsies (3):
- Abnormal movements, such as twitching or jerking, due to temporary irregularities in muscle movements and muscle tone, limpness, or stiffness accompanied by loss of consciousness and noisy or shallow breathing
- Changes in behavior such as not responding when addressed
- Spells of staring blankly into space or appearing confused or scared
- Abnormal behaviors such as automatic movements, including chewing, swallowing, or picking at clothing
- Sensory disturbances such as changes in vision, smell, or hearing; feeling tingly or numb; or experiencing unusual feelings that are hard for the child to describe
Some signs and symptoms may be visible while some may not. It is recommended to seek medical care to evaluate any complaints since many cases go unnoticed until complications occur.
Complications Of Epilepsy In Children
Epilepsy may increase the risk for learning and mood disorders in some children and result in physical conditions such as ulcers and headaches (4). In addition, an epilepsy or seizure can have life-threatening complications (5)
- Falling during seizures increases the risk of fractures and head injuries.
- Drowning risk can be 15 to 19 times higher in children due to seizures while bathing or swimming.
- Psychological problems, such as depression, anxiety, and suicidal thoughts, may be caused by the condition or side effects of epilepsy medications.
Although rare, the following life-threatening complications may occur in some children (5):
- Status epilepticus: In this condition, seizures last for more than five minutes, or recurrent seizures occur without gaining consciousness between them, causing permanent brain damage in some cases.
- Sudden unexpected death in epilepsy (SUDEP): It appears in one percent of epilepsies. Heart or respiratory conditions are believed to cause it, but the exact cause is unknown.
Diagnosis Of Epilepsy In Children
Epilepsy is diagnosed if a seizure occurs more than once without known causes such as brain injury or fever. Children who have such unprovoked seizures need emergency medical care.
The following steps comprise the diagnostic process of epilepsy(4):
- Detailed medical history, including family history, pregnancy and delivery history, previous head injuries, and infections, is obtained. Doctors may also ask about specific symptoms and the details of the seizures.
- Physical examinations, including neurological, cardiac, and mental assessments, are conducted.
- Blood tests are often ordered to identify any potential causes of illness.
- Magnetic resonance imaging (MRI) or computed tomography (CT) scans are ordered to visualize the brain tissue and identify injuries and structural damages to the brain structures.
- Electroencephalogram (EEG) helps to record the electrical activity of the brain in the waveform. It may help determine the seizure type, epilepsy syndrome, location, and risk of recurrence (5).
After these exams and tests, the doctors may observe the child for other symptoms, such as seizures, to confirm the diagnosis.
Treatment For Epilepsy In Children
There is no right treatment or dosage that fits all children since epilepsy is a complex condition. Pediatric neurologists may recommend medications and other treatments based on the type of epilepsy and other individual factors.
The common epilepsy treatments may include (4)
- Anti-epilepsy drugs (AEDs)
These are also called anti-seizure drugs or anticonvulsant drugs and help prevent seizures. Anti-epilepsy drugs do not cure the underlying brain pathology; they only reduce the recurrence and frequency of seizures. Many types of AEDs are available, and it may take a while to know which medication helps your child best.
Epilepsy medications may also not work until they reach a certain level in the blood. Hence, doctors may gradually change the dosage or drugs based on the response. Under the doctor’s supervision, some children may gradually be put off medication if they don’t develop seizures for a few years.
If there is no improvement with medication, the following treatment options may be considered for children with epilepsy (5):
- Dietary therapy
A ketogenic diet, modified Atkins diet, or low glycemic index diet is recommended for children with epilepsy. Some notice a lower frequency of seizures while adhering to strict low-carb diets.
The ketogenic diet, a high-fat and low carbohydrate diet, is primarily recommended. Other diets are recommended if it is not possible to follow a keto diet. However, these diets can have certain side effects, such as constipation and nutritional deficiencies. Hence, seek the guidance of a pediatrician dietician to avoid these problems in your child.
- Brain surgery
Surgery is recommended if mediations and dietary interventions fail to control seizures. The surgery may involve removing the brain areas causing seizures if it originates from a small, well-defined area. The removal is only done if it does not interfere with vital body functions, including vision, movements, hearing, and speech.
Children who undergo epilepsy surgery may be at risk of surgical complications, such as cognitive impairments, and require medical therapy.
- Medical devices
Medical devices, such as vagus nerve stimulators, are implanted in the skin to control seizures. Deep brain stimulations are also done with electrodes. However, children need to take anti-epileptics along with device therapy.
Epilepsy is considered to be resolved if a child having age-dependent epilepsy passes the applicable age or remains seizure-free for ten years with medication or five years without medication (1). Adhering to long-term treatment is necessary for epilepsy. Some promising treatments, such as responsive neurostimulation with pacemaker-like devices, external stimulator devices, minimally invasive surgeries, and laser ablation, are in the process of trials (5).
Prevention Of Epilepsy In Children
According to the World Health Organization (WHO), nearly 25% of epilepsy cases are preventable. The WHO recommends the following steps to prevent epilepsies (6):
- Ensure adequate perinatal care to lower new epilepsy cases due to birth injuries.
- Use fever medications to lower fever in children before they develop febrile seizures.
- Prevent head injuries to avoid post-traumatic epilepsy.
- Prevent central nervous system infections, such as neurocysticercosis, by avoiding uncooked or undercooked meats.
Using safety equipment, such as helmets, during sports can prevent head injuries in many children. Furthermore, getting childhood immunizations on time could also prevent certain infections that can lead to brain damages.
Helping Your Child Cope With Epilepsy
Parental understanding of the condition helps many children. You may contact emergency care and do the following while your child is having a seizure (5):
- Place something soft, such as a cloth or pillow, under their head
- If possible, roll the child to one side
- Loosen tight clothing, especially around the neck
- Keep dangerous objects away if the child is moving and ensure they won’t fall off if they are on a bed
- Do not restrain the child
- Do not put your fingers or anything else in their mouth
Try to stay calm and observe the seizure until the emergency help arrives so that you can explain it to the doctor. In addition, you may do the following steps to avoid or reduce the risk of recurrent episodes of epilepsy symptoms (5):
- Give medications as prescribed and change medications only after discussing with the doctor.
- Make them wear a medical alert bracelet since this may help paramedics know if the child has a seizure outside the home.
- Ensure enough rest and good sleep for children since inadequate sleep may trigger seizures.
- Encourage them to exercise since this may promote physical and mental health in children.
- Explain the condition to peers and teachers and tell them what to do if the child develops a seizure episode while at school or outside.
- Keep written details about the child’s condition, medication, and treating doctor, in their bags or wallets so that it is easily available.
In addition to this, ensuring the safety of children with seizures is also essential to prevent injuries. For example, do not leave them unattended while swimming or bathing, and avoid letting them sleep on bunk beds. You may also seek support from epilepsy support groups for positive encouragement.
Types Of Epilepsy In Children
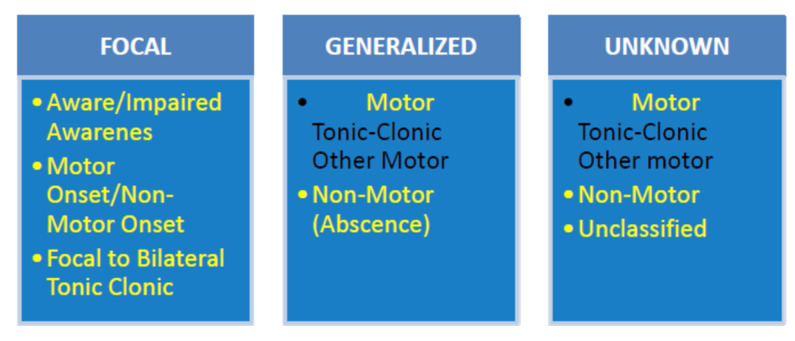
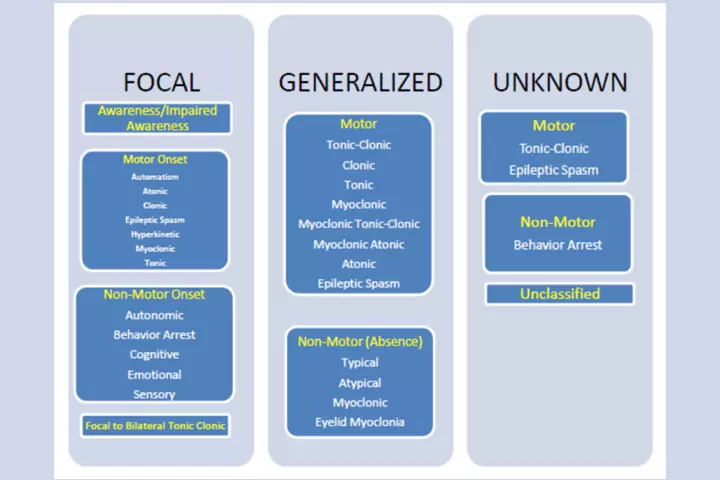
Epilepsies can be classified into various groups depending on the cause, type of seizure, affected brain area, age of onset, and pattern of EEG waves. Seizures are broadly classified into the following types (7):
- Generalized seizures
Generalized seizures may occur if both brain hemispheres are affected and can be of the following types:
- Absence seizures or petit mal seizures with rapid eye blinking or short staring spells
- Tonic-clonic seizures or grand mal seizures with specific muscle movements and spasms with a loss of awareness.
- Focal seizures
Focal seizures or partial seizures occur due to abnormal electrical activity in a specific brain area and may include
- Focal aware seizures affecting small areas of the brain and causing usual movements or sensations
- Focal unaware seizures with random movements and loss of awareness for a few seconds
ILAE 2017 Classification of Seizure Types: Basic Version
ILAE 2017 Classification of Seizure Types: Expanded Version
Some children with recurrent and frequent seizures may have epilepsy syndromes. These are groups of signs and symptoms of epilepsy occurring at a particular age. The characteristics and symptoms of childhood epilepsy syndromes vary depending on the type.
The following types of epilepsy syndrome or epilepsy are common in children (8) (9):
- Childhood absence epilepsy (CAE) can occur between ages two and 12 and causes brief absence seizures. Children may continue to do what they were doing after the seizure. It can be controlled with anti-epileptics and often resolves in puberty.
- Juvenile absence epilepsy (JAE) occurs between ages eight and 12 and involves longer absence seizures and movements, such as chewing or fluttering eyelids. Tonic-clonic seizures are also seen in 80% of children with JAE. Although it can be managed with medications, it is a lifelong condition.
- Temporal lobe epilepsy (TLE) can begin at any age and comprises focal onset seizures with unusual behaviors and emotions and confusion with or without loss of consciousness. In some children, TLE may progress into tonic-clonic seizures in the future.
- Frontal lobe epilepsy (FLE) comprises focal onset seizures occurring at any age. It may impair motor activities or emotions with or without altered awareness and may often be confused with behavioral and psychiatric issues in children.
- West syndrome or infantile spasms is a type of epilepsy typically occurring in the first year of life. It causes brief spasms that make the infant stiff. These spasms may occur in clusters, and babies may cry, causing it to be misidentified as colic. Babies with infantile spasms are at risk of developing intellectual disabilities and Lennox-Gastaut syndrome in childhood.
- Lennox-Gastaut syndrome (LGS) is an epilepsy syndrome with onset between ages three and five. Up to 90% of children with this condition have intellectual disabilities. It may cause various seizure types and often does not respond to medical therapy.
- Benign rolandic epilepsy, also called benign epilepsy with centrotemporal spikes (BECTS), may occur between ages one and 14. Focal seizures with movements are seen in this condition. Children may also have speech problems and drooling. However, medical treatment is not required in many cases as it resolves by age 15.
- Juvenile myoclonic epilepsy (JME) has an onset between ages eight and 25 and causes myoclonic seizures in the morning or after walking. It often runs in families and can be controlled with medications and lifestyle changes.
- Dravet syndrome (DS) is a severe myoclonic epilepsy often seen in infancy, and it continues lifelong. It is triggered by high body temperatures such as from fever or hyperthermia (10).
- Doose Syndrome, also known as myoclonic-astatic epilepsy (MAE), is seen in children aged one to five and appears without a known cause. It may cause children to fall to the ground, often resulting in injuries due to abrupt loss of muscle control.
- Rasmussen’s syndrome causes seizures due to brain inflammation (Rasmussen’s encephalitis) affecting one hemisphere.
- Genetic epilepsy with febrile seizures plus (GEFS+) is an epilepsy syndrome often seen in children with family members having various epileptic seizures and epilepsy syndromes. These epileptic seizures begin with febrile convulsions, and certain genetic mutations are known to cause them.
- Landau-Kleffner syndrome (LKS) causes aphasia (language impairment) with seizures in children.
You may ask your pediatrician what type of epilepsy your child has to understand it better. Always remember that a single episode of seizure or seizures with certain causes is not diagnosed as epilepsy.
Frequently Asked Questions
1. Can a child outgrow epilepsy?
Epilepsy may be temporary for some children who eventually outgrow this neurological problem. For others, the disorder may persist a lifetime (11).
2. Can a child with epilepsy go to a normal school?
Yes, most children with epilepsy can attend school and participate in sports and other activities under appropriate supervision. However, parents should inform the school about their child’s condition so that they can help the child if the need arises (12).
3. Is epilepsy considered a disability?
The Americans with Disabilities Act covers people with epilepsy. Hence, the disorder is considered a disability (13).
Epilepsy is a complex disorder requiring long-term treatments and, often, lifelong medications. Therefore, it is important to identify and treat the condition as early as possible to prevent worsening or complications. Adhering to treatments and regular follow-ups are essential in epilepsy care.
Key Pointers
- Structural brain damage, genetic conditions, and genetic changes can cause epilepsy in kids.
- High temperature, mental disability, and premature birth increase the risk of this disease.
- Epilepsy also exposes children to dangers, such as falling, drowning, and psychological problems.
- Adequate perinatal care, fever medications, and precluding head injuries can help prevent epilepsy.
- If your child has a seizure, placing a cloth or pillow below their head, rolling them to one side, and loosening clothing around their neck could help.
References
Articles on thebridalbox are backed by verified information from peer-reviewed and academic research papers, reputed organizations, research institutions, and medical associations to ensure accuracy and relevance. Read our editorial policy to learn more.
- Carmelo Minardi et al; (2019); Epilepsy in Children: From Diagnosis to Treatment with Focus on Emergency.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6352402/ - Causes of epilepsy.
https://epilepsysociety.org.uk/about-epilepsy/what-epilepsy/causes-epilepsy - Epilepsy.
https://www.rch.org.au/kidsinfo/fact_sheets/Epilepsy_an_overview/ - Epilepsy in Children: Diagnosis & Treatment.
https://www.healthychildren.org/English/health-issues/conditions/seizures/Pages/Epilepsy-in-Children-Diagnosis-and-Treatment.aspx - Epilepsy.
https://www.stclair.org/services/mayo-clinic-health-information/diseases-and-conditions/CON-20117122/ - Epilepsy.
https://www.who.int/news-room/fact-sheets/detail/epilepsy - Types of Seizures.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/epilepsy/types-of-seizures - Epilepsy In Children.
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/epilepsy-in-children - Epilepsy Syndromes In Children.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/epilepsy/epilepsy-syndromes-in-children - Dravet Syndrome.
https://rarediseases.org/rare-diseases/dravet-syndrome-spectrum/ - Epilepsy in Children and Teens.
https://www.yalemedicine.org/conditions/pediatric-epilepsy# - Epilepsy Factsheet (for Schools).
https://kidshealth.org/en/parents/epilepsy-factsheet.html - Americans With Disabilities Act: An Overview.
https://www.epilepsysandiego.org/resources/legal-issues/#

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Neema Shrestha
Read full bio of Aastha Sirohi