Chorioamnionitis: What Is It And How Is It Treated
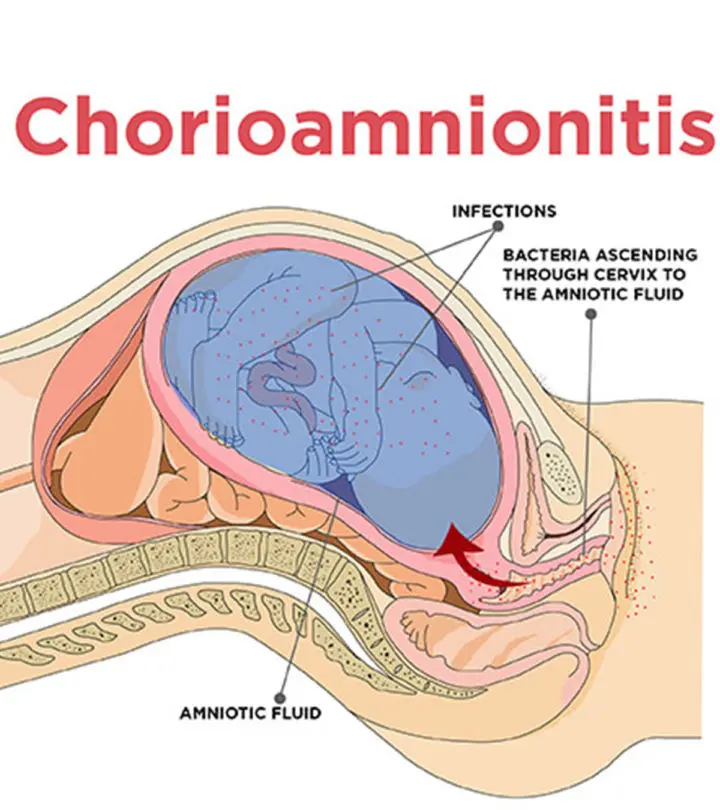
Image: Shutterstock
Chorioamnionitis is a pregnancy complication associated with weakened immunity and delicate state of health. Typically, it is experienced in the later phases of pregnancy, when the fetal membranes rupture during labor.
Though not a life-threatening condition, if not treated on time, chorioamnionitis can lead to complications for the mother and the baby, before and after delivery.
MomJunction will tell you more about chorioamnionitis, its causes, risks, treatment, and ways to prevent it.
In This Article
What Is Chorioamnionitis?
Chorioamnionitis is an acute bacterial infection affecting the fetal chorion (outer membrane), amnion (fluid-filled sac) and amniotic fluid (in which the fetus floats). It occurs during pregnancy or labor and leads to severe infections in the mother and the baby.
Chorioamnionitis affects one to four percent births in the US and in most cases, the fetus needs to be delivered as soon as possible, sometimes resulting in preterm birth (1).
It is also referred to as amnionitis (inflammation of the amnion), chorionitis (inflammation of the chorion), amniotic fluid infection, intra-amniotic infection (IAI), intrauterine infection and intrapartum infection.
What Are The Causes Of Chorioamnionitis?
Chorioamnionitis is commonly caused due to Group B streptococci, E.Coli, and anaerobic bacteria (1).
The infection develops when the bacteria, usually present in the lower genital tract, ascend and infect the amniotic sac. This leads to a bacterial infection in the amniotic fluid, placenta, and the fetus.
What Are The Risk Factors For Chorioamnionitis?
Certain risk factors increase the chances of contracting chorioamnionitis. Some of them are (1):
- First pregnancy
- If the membranes (chorion and amnion) surrounding the fetus rupture (while water breaking) for an extended period
- Multiple unsterile vaginal examinations during labor
- Frequent internal monitoring of the uterus and fetus
- Pre-existing infections of the lower genital tract. These infections include group B strep infection and bacterial vaginosis
- Sexually transmitted infections
- Meconium-stained amniotic fluid
- Reduced functioning of the immune system in the mother or fetus
- Smoking, alcohol and drug abuse
- African-American ethnicity
What Are The Symptoms Of Chorioamnionitis?
Usually, chorioamnionitis will not show any symptoms, which makes it difficult to detect the condition until you go for a checkup. However, some women with a severe infection will show the following signs and symptoms (2):
- High grade fever and sweating
- Rapid heartbeat in the mother and fetus
- Painful or tender uterus
- Foul smelling vaginal discharge that is amniotic fluid
These symptoms may also indicate other medical conditions. Therefore, it is better to consult your healthcare provider for a more accurate diagnosis.
How Is Chorioamnionitis Diagnosed?
A clinical diagnosis (complete physical examination), and pathological diagnosis (laboratory tests for examining the placenta) are needed to diagnose chorioamnionitis (1)
Clinical diagnosis
To begin with, doctors check for symptoms of chorioamnionitis. If you have the symptoms discussed above, a thorough physical examination is conducted to make a concrete diagnosis. The treatment begins immediately in such cases.
Otherwise further tests are recommended for diagnosing the condition. However, if you have already reached the full term of your pregnancy, the doctor will not perform any further diagnostic tests.
Pathological diagnosis
The additional tests to rule out chorioamnionitis include:
- Testing for maternal leucocytosis, where white blood cell count of >12,000/mm3 or >15,000/mm3 is an indication of IAI. A positive diagnosis for leucocytosis, in the absence of other signs and symptoms, may be due to conditions such as labor and steroid use.
- Blood tests for checking high levels of C-reactive protein (CRP), soluble intercellular adhesion molecule 1 (SICAM1), Lipopolysaccharide binding protein (LBP) and Interleukin 6 that are associated with a higher risk of amnionitis.
- Amniotic fluid testing that checks for low concentration of sugars and high levels of blood cells and bacteria.
- Histological examination of the placenta and umbilical cord to check for alterations in the amniotic membrane and placental chorion.
What Are The Complications Of Chorioamnionitis?
If you have a severe case of chorioamnionitis, or when the condition is left untreated, it can cause complications for both the mother and the baby (1).
Maternal complications
- Miscarriage or stillbirth
- Preterm labor
- Pelvic or abdominal infections
- Endometriosis
- Heavy postpartum bleeding
- Blood clotting in the pelvis and lungs
- Pelvic abscess (pus in the pelvis)
- Bacteremia (bacterial infection in the bloodstream)
- Septic shock (life-threatening blood infection)
Fetal/ newborn complications
- Meningitis (infection of the membranes surrounding the brain and spinal cord)
- Cerebral palsy and brain injury
- Respiratory issues
- Bacteremia
- Pneumonia
- Intrauterine fetal demise (death of the baby in the uterus)
- Chronic lung disorder
- Neonatal sepsis (bacterial bloodstream infection in the newborn)
Immediate treatment will reduce the chances of complications in the mother and also protect the baby from getting infected.
How Is Chorioamnionitis Treated?
The course of treatment for chorioamnionitis depends on the duration of your pregnancy, and the time that the baby needs for development (3).
Antibiotic treatment
Antibiotics are safe for the mother and the fetus. They interfere with the bacterial wall and prevent it from multiplication. But they are usually the last resort since over usage of these medications can make the bacteria resistant to drugs (4).
- Gentamicin, metronidazole and amoxicillin are primarily prescribed.
- If you are allergic to penicillin, the doctor will use an alternative antibiotic – clindamycin.
- Sometimes, broad-spectrum antibiotics such as cefoxitin, cefepime, piperacillin-tazobactam and cefotetan are used to treat chorioamnionitis.
Usually, you will be given these antibiotics intravenously until you deliver or show no symptoms for 24 hours. This is an in-hospital treatment, and you are allowed to go home when the signs of the infection disappear.
Surgical intervention
- Immediate delivery is the option in the case of severe chorioamnionitis or if you have reached full-term.
- Oxytocin is given for inducing labor if the condition causes uterine atony (loss of uterine muscle tone)
Your doctor will go for cesarean delivery in the following cases:- Prolonged vaginal delivery
- Your condition is deteriorating
- There are signs of fetal distress
Supportive care (in case of neonatal sepsis)
The newborn is:
- Kept for observation in the NICU or on a ventilator
- Treated for hypovolemia (reduced blood circulation), respiratory distress and metabolic acidosis (the condition where kidneys do not flush enough acid)
- Treated for thrombocytopenia (platelet deficiency) or coagulopathy
- Glucose homeostasis (regulation of blood sugars)
Use of herbal or natural remedies may sometimes aid in treating the condition more effectively.
Natural Remedies For Chorioamnionitis
Natural remedies may or may not treat the infection, but they can boost the immune system and support the antibiotics in fighting the infection. Some of the commonly used natural or herbal remedies are:
- Raw garlic: Garlic is traditionally used to treat vaginal infections. Mince two to four cloves and allow it to sit for some time so that the allicin component (the antibacterial agent) gets activated. Then, you can either add it to your salad or swallow it with water (5).
- Echinacea: This herb is known to improve immunity, and thereby effectively fight infections (6). Therefore, it can be used for fighting the bacterial infection of chorioamnionitis. However, there is no concrete evidence to substantiate this claim; so make sure you take this herb under the supervision of your OB/GYN.
- Astralagus: It is a traditional Chinese medicinal herb known for immunological properties (7). You can add some of this herb to rice or soup and savor it. However, you should note there is no scientific study to understand the safety of this herb during pregnancy.
- Probiotic diet: Consuming fermented foods such as curd and yogurt every day can be useful in treating the bacterial infection (8).
How Can Chorioamnionitis Be Prevented?
Your doctor will tell you about the measures to take to prevent chorioamnionitis. The methods used to screen and prevent chorioamnionitis include:
- Screening for bacterial vaginosis in the later part of the second trimester
- Testing for Group B streptococcal infections between the 35th and 37th week of pregnancy
- Reducing the frequency of vaginal examinations during labor
- Minimizing the number of internal investigations
Also, you should be going for regular checkups to address your concerns and queries.
Frequently Asked Questions
1. Can you get pregnant after chorioamnionitis?
Yes, you are most likely to get pregnant after chorioamnionitis, but with a two-fold risk of acquiring the infection in the subsequent pregnancies (9).
2. What is the difference between chorioamnionitis and endometritis?
Chorioamnionitis is the inflammation of the fetal membranes (amnion and chorion) whereas endometritis is the inflammation of the endometrium (inner lining of the uterus), although both occur due to infections.
Chorioamnionitis afflicts many pregnant women across the world, typically when the woman has prolonged labor or protracted membrane rupture. Based on certain clinical symptoms, such as maternal fever, histological testing of the placenta and umbilical cord, and positive results in amniocentesis, doctors can diagnose the presence of the infection.
Antibiotics help treat the infection successfully and also play a vital role in preventing maternal and fetal complications.
Have you been diagnosed with chorioamnionitis? What were your experiences during your pregnancy? We would love to hear from you. So, feel free to comment on this article.

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.