6 Types Of Congenital Heart Disease In Children, Signs & Causes
The symptoms often become evident in the first few months after birth.
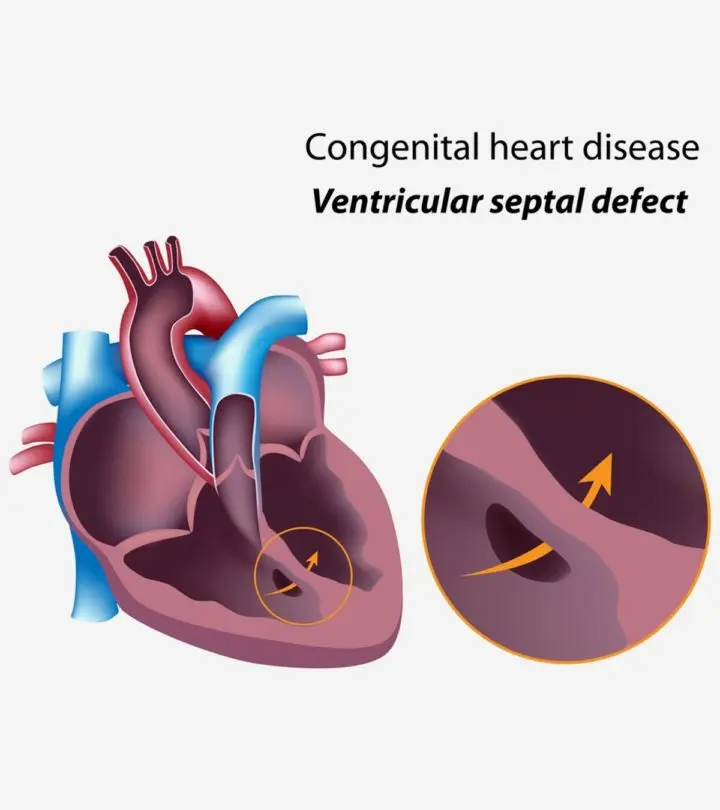
Image: Shutterstock
In This Article
Congenital heart disease in children is a structural heart defect present at birth. The condition is also called congenital heart anomaly or defect. Congenital heart disease or CHD could impact any part of the heart. The defects may affect the heart’s functions adversely. CHDs may be characterized by small holes that usually heal independently, a missing portion in the heart, or an underdeveloped part. The diagnosis and treatments may vary as per the type of heart defect and the child’s age when the condition is diagnosed. This post will help you learn about congenital heart defects in children, including their causes, symptoms, and treatments.
Signs And Symptoms Of Congenital Heart Diseases
The onset of signs and symptoms may occur immediately after birth or during the first few months of life in children with severe congenital heart defects. The signs and symptoms could include the following (1).
- Rapid breathing
- Shortness of breath, especially during feeding
- Inadequate weight gain
- Cyanosis (bluish or pale gray skin)
- Leg edema (swelling)
- Orbital edema (swelling around eyes)
- Abdominal swelling
- Sweating
Babies with the above-listed symptoms may require a medical evaluation to identify the cardiac defects. Less severe congenital heart diseases can be asymptomatic in early life years. The following symptoms and signs in childhood may indicate cardiac defects.
- Shortness of breath while exercising or during other physical activities
- Syncope or fainting during physical exertion
- Quickly becoming tired on exertion
- Ankles and hand edema (swelling)
Exercise intolerance and swelling of extremities in children require medical care. Children may not develop other signs and symptoms until the condition worsens. Restricting physical activities do not cure the disease. Instead, seek pediatric care at the earliest.
Causes And Risk Factors For Congenital Heart Diseases
The exact cause may not be identified for all types of heart defects present at birth. However, fetal heart development problems are the leading cause of congenital heart defects (2). Genetic and environmental factors may increase the risk of developing congenital heart defects. Children with affected close relatives may have an increased risk for heart defects.
The following factors during pregnancy may also lead to problems in fetal heart development (3).
- German measles (rubella) infections
- Uncontrolled maternal diabetes during pregnancy
- Alcohol use
- Cigarette smoking and use of other tobacco products
- Certain medications, such as ACE inhibitors, statins, and thalidomide
Avoiding risk factors before pregnancy may reduce the risk of heart problems in some children. Parents with already affected children may seek genetic counseling before planning the next child.
Types Of Congenital Heart Defects
There are various types of heart defects (2).
1. Holes in the heart
Heart development issues may leave holes in the walls of heart chambers (atria and ventricles) or on major blood vessels. These holes may cause mixing of oxygenated blood and deoxygenated blood from both sides of the heart and cause oxygen insufficiency in the body and congestive heart failure.
The following defects occur due to holes in the heart or major blood vessels.
- Ventricular septal defect (VSD) is a hole in the ventricular septum (wall between the ventricles).
- Atrial septal defect (ASD) is opening in the atrial septum (wall between the atria).
- Complete atrioventricular canal defect is a hole in the heart’s center connecting all chambers of the heart.
- Patent ductus arteriosus (PDA) is opening between the pulmonary artery and aorta, causing mixing of the well and poorly oxygenated blood.
- Patent foramen ovale (PFO) is an opening in between the atrial wall; PFO can be smaller than the atrial septal defect hole and often resolves itself.
2. Obstructed blood flow
Blood flow may be obstructed in defects causing narrowing or blockage of major blood vessels or heart valves. In such conditions, the heart may work more to pump blood and often result in the thickening of the heart muscles (cardiac hypertrophy) and heart enlargement (cardiomegaly).
Heart defects obstructing blood flow may include:
- Pulmonary stenosis is the narrowing of the pulmonary valve, blocking normal blood flow to the lungs.
- Aortic stenosis is the narrowing of the aortic valve, obstructing blood flow to the body.
3. Abnormal blood vessels
Abnormalities in the formation of major blood vessels could affect the blood supply. Such defects may include:
- Transposition of the great arteries occurs when the aorta and pulmonary artery are developed on the reverse sides of the heart.
- Coarctation of the aorta is a condition where the aorta is too narrow and fails to supply enough blood.
- Vascular rings are the malformation of the aortic arch, which encircle the trachea and food pipe, causing breathing issues or feeding difficulties.
- Total anomalous pulmonary venous connection is the misplaced attachment of blood vessels from the heart.
- Truncus arteriosus is when a common blood vessel supplies blood to the lungs and the body instead of a separate aorta and pulmonary artery.
4. Heart valve abnormalities
Abnormalities of heart valves may affect the blood flow. Various anomalies can cause opening or closing issues of valves, resulting in backflow or insufficient blood flow.
- Congenital mitral valve anomalies may include various types of defects, such as an increased thickness of the valve leaflets, abnormalities of the heart muscle where the valve is attached, and anomalies in the cords that support the valve. These issues may result in mitral stenosis, regurgitation, or prolapse in some children.
- Ebstein anomaly is a malformation of a tricuspid valve (between the right atrium and right ventricle), causing a leak of blood.
- Pulmonary atresia is the absence of a pulmonary valve, causing abnormal blood flow to the lungs.
- Tricuspid atresia occurs when the valve between the right atrium and ventricle is not formed. The blood flow to the right ventricle can be obstructed by a solid tissue at the valve’s place, often resulting in the underdevelopment of the right ventricle.
- Bicuspid aortic valves only have two valve leaflets instead of three. This may affect the normal blood flow. and cause regurgitation of the blood.
5. Underdeveloped heart
Some children may have underdeveloped parts or portions of the heart. A common issue is hypoplastic left heart syndrome, where the left side of the heart is underdeveloped and fails to pump sufficient blood to the body.
6. Combination of defects
Some children may have a combination of several heart defects. This can be more severe than single defects and often require immediate interventions. Tetralogy of Fallot is a combination of four heart defects, including a ventricular septal defect (VSD), pulmonary valve stenosis, right ventricular hypertrophy (thickened right ventricular muscles), and a misplaced aorta.
Complications Of Congenital Heart Defects
Potential complications of congenital heart defects may include the following (4).
- Delayed growth and development are seen in children with congenital heart diseases.
- Cyanosis may be seen in babies with shunting of oxygen-rich and oxygen-poor blood in the heart chambers.
- Congestive heart failure may occur in major heart defects where the heart cannot pump enough blood.
- Stroke may occur due to complete or partial interruption of blood supply to a part of the brain.
- Abnormal heart rhythms or arrhythmias may occur due to heart defects.
Children with congenital heart defects may require lifelong follow-up visits even after correction to avoid the risk of valve problems, endocarditis, heart failure, and other heart problems.
Prevention Of Congenital Heart Defects
Prevention may not be possible in all cases since some children may develop heart defects without known causes. However, the following ways may help to reduce the risk of congenital heart defect in some children (5).
- Seek preconception care or early prenatal care
- Get the German measles (rubella) vaccine before planning pregnancy
- Discuss with doctors and choose pregnancy-safe medications
- Avoid OTC drugs and self-treatment during pregnancy
- Avoid the use of alcohol, tobacco, and narcotics during pregnancy
- Take vitamin and iron supplements as recommended
- Eat healthily and exercise as per recommendations
Heart development happens in the early weeks of pregnancy, so it is advisable to seek preconception care and follow healthy habits before conception.
Diagnosis Of Congenital Heart Defects
The doctor could conduct a physical examination to determine the signs and heart murmurs that may indicate cardiac issues. Some children may already be diagnosed with congenital heart defects from a fetal echocardiogram or other tests during infancy. Although the anomaly is present from birth, a few children may have late onset of symptoms.
The following tests are ordered to confirm the diagnosis (6).
- An electrocardiogram or ECG records the electrical activity of the heart. This may help identify rhythm abnormalities. Echocardiograms also help visualize the structures and evaluate the heart chambers and valves’ function.
- Pulse oximetry may help to determine the oxygen levels in the blood. This can also be used as a screening tool in the newborn nursery.
- Chest X-rays help to visualize heart size and extra fluid in the lungs.
- Cardiovascular MRI may help to visualize heart defects in older children.
- Cardiac catheterization may also provide detailed visualization of the heart and it’s vessels.
Doctors may also order genetic testing and blood tests to determine any underlying causes based on the existing signs and symptoms.
Treatment For Congenital Heart Defects
The treatment options may vary depending on the heart defects’ type and severity. Some congenital heart defects, such as a tiny ventricular septal defect, may disappear without any treatment. A few conditions may require elaborate treatments to prevent complications.
The following treatments are usually given for congenital heart defects (7).
- Cardiac procedures through catheterization help repair some defects without surgically opening the chest cavity and the heart. This uses tiny, flexible tubes guided with X-ray images to reach the heart and correct the defect.
- Open heart surgery by making a chest incision is required to correct significant defects.
- Placement of artificial cardiac pacemakers and implantable cardioverter defibrillators (ICD) is often necessary to correct rhythm abnormalities.
- Medications, such as ACE inhibitors, diuretics, ARBs, and antiarrhythmic drugs, are often prescribed for mild heart defects
- Heart transplantation is recommended for children with severe unrepairable defects.
A combination of treatments is often needed for some defects. Some children may receive medications, while surgery may be delayed for the future. Catheter procedures and surgeries may be done in steps over the years, depending on the requirements.
Frequently Asked Questions
1. What is the life expectancy for a child with a congenital heart defect?
The survival rate of a child with congenital heart defects depends on the type and treatment. Although it is generally estimated that they may survive upto one year of adulthood, some can even live as long as other healthy individuals. Therefore, life expectancy may vary based on lifestyles and treatments over time (8) (9).
2. Can CHD be cured?
No, congenital heart defects are not curable. There may be correction treatments for the heart, but it is not completely cured and may result in long-term effects (10).
3. Is congenital heart disease fatal?
Congenital heart diseases must be treated upon diagnosis, but the most severe type, i.e., critical congenital heart disease, can become fatal upon delay or no treatment (11).
4. What is the most common congenital heart disease found in children?
The ventricular septal defect is the most common type to affect children (8).
Congenital heart disease in children may manifest as holes in the heart, obstructed blood flow, or an underdeveloped heart. Your child may show shortness of breath, cyanosis, and leg edema. You may not be able to identify the exact cause of this condition, but uncontrolled maternal diabetes during pregnancy, cigarette smoking, and alcohol maybe some of the risk factors. If you notice some worrying symptoms of CHD in your child, seek a doctor’s advice. After a complete diagnosis, they may suggest treatments based on the results. CHD in children requires lifelong treatment and follow-up. However, with better treatment options, the quality of life can be improved.
Key Pointers
- Shortness of breath, bluish or gray skin tone, and swollen legs could be signs of congenital heart disease in children.
- Smoking, alcohol consumption, or rubella infections during pregnancy could cause congenital heart disease in babies.
- Doctors may diagnose the heart defect using an ECG or a chest X-ray.
- The treatment plan may include diuretics, heart surgery, or the use of pacemakers.
References
2. Congenital Heart Disease; Lucile Packard Children’s Hospital, Stanford
3. Congenital Heart Disease in adults; St. Clair Health
4. Complication; Congenital Heart Disease; National Health Service
5. Prevention; Congenital Heart Disease; National Health Service
6. Symptoms and Diagnosis of Congenital Heart Defects; American Heart Association
7. Care and Treatment for Congenital Heart Defects; American Heart Association
8. Data and Statistics on Congenital Heart Defects; Centers for Disease Control and Prevention
9. Graham J.Reid et al. (2006); Estimates of Life Expectancy by Adolescents and Young Adults With Congenital Heart Disease; Science Direct
10. Can You Be Cured of Congenital Heart Disease? Nationwide Children’s
11. CONGENITAL HEART DEFECTS AND CRITICAL CHDS; March Of Dimes

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Elham Raker