DVT In Pregnancy: Risks, Symptoms, Prevention And Treatment
DVT in pregnant women is not uncommon and may cause severe side effects.
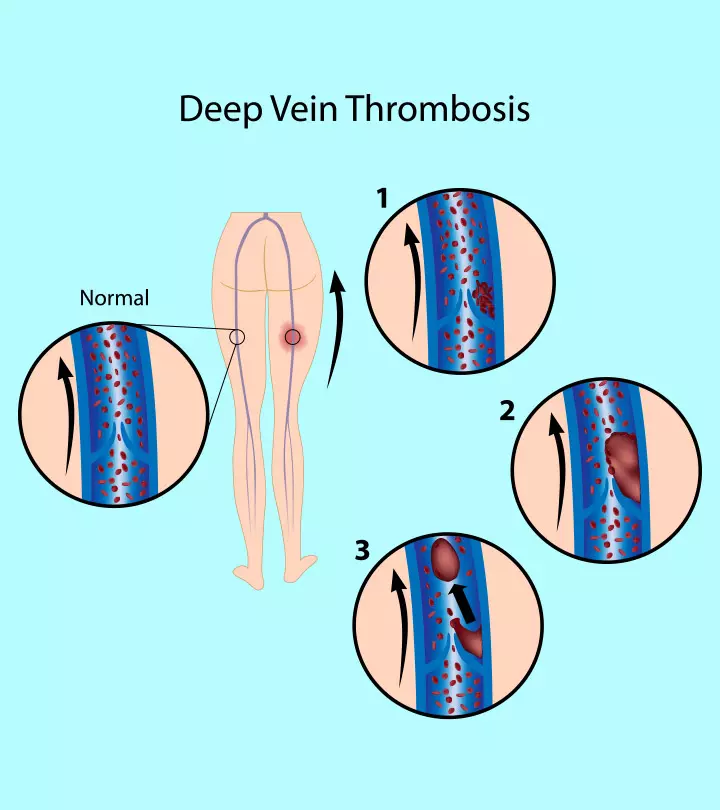
Image: Shutterstock
In This Article
When a blood clot develops in the body’s deep veins, mainly in the leg, calf, or pelvis, causing pain and swelling, it is called deep vein thrombosis (DVT). DVT in pregnancy is uncommon; hence, pregnant women often undermine swelling or pain in the legs or feet as a muscle cramp caused by pregnancy-induced changes, such as weight gain.
However, pregnant women are five times more likely to develop a blood clot (1). Further, DVT is the most common venous thromboembolism (VTE) and can adversely affect the mother’s health.
Read this post to know more about DVT and its symptoms, risk factors, complications, diagnosis, treatment, and prevention in pregnant women.
Symptoms Of DVT In Pregnancy
The most common symptom of DVT in pregnant and postpartum women is discomfort and swelling in the left lower extremity veins. However, some pregnant or early postpartum women present no symptoms, known as “silent DVT” (2).
The clinical symptoms of DVT in pregnancy include (2) (3)
- Unilateral (one-sided) leg pain and swelling
- Difficulty walking
- Erythema (redness) of the affected leg
- Warmth in the affected area
- Isolated iliac vein thrombosis with abdominal pain, back pain, or swelling of the limb
Risk Factors For DVT In Pregnancy
DVT may occur during pregnancy or within the first six months of the postnatal period. However, certain risk factors may predispose pregnant women to develop DVT, including (2) (3)
- Inherited or acquired thrombophilias (familial history of venous thrombosis)
- Personal history of thrombosis
- Antiphospholipid syndrome
- Medical conditions such as lupus, heart disease, arthritis, cancer, and sickle-cell anemia
- Pregnancy at 35 years or above (advanced maternal age)
- Multiple gestations (e.g., twins or triplets)
- Multiparity (three children and above)
- Obesity and lack of movement
- Gestational diabetes
- Pre-eclampsia
- Assisted reproduction
- Dehydration
- Hospitalization for non-delivery reasons
- Systemic infections
- Prolonged immobility such as while traveling for long hours or during bed rest
- Smoking and using intravenous drugs
- History of painful varicose veins or ones above the knee with redness/swelling
The risk factors of developing DVT in the postpartum period include (2) (3)
- Preterm delivery
- Stillbirth
- Postpartum infection
- Preeclampsia
- Long labor of more than 24 hours
- Operative vaginal delivery
- Cesarean delivery
- Blood transfusion following childbirth due to extreme blood loss (postpartum hemorrhage of over one liter)
Complications Of DVT In Pregnancy
Pregnancy is a prothrombotic state (tending to promote blood clots) that develops to prevent excessive blood loss during childbirth or miscarriage (2). Therefore, the risk of developing a DVT is higher in pregnancy though it is uncommon. If untreated, DVT could result in the following pregnancy complications:
- Pulmonary embolism (PE) is the leading cause of maternal death in the US. It occurs when a deep vein thrombotic clot breaks off and moves into the lungs (1).
- Post-thrombotic syndromes (PTS), such as chronic (persistent) leg pain, intractable edema, and leg ulcers, are caused by incomplete recanalization or permanent damage to the venous valves. They result in valvular reflux, further increasing the morbidity and mortality of DVT (2).
Early diagnosis and appropriate treatment of DVT during pregnancy can help prevent PE and PTS.
DVT does not have detrimental effects on the baby unless serious complications exist. However, the available treatment options for DVT during pregnancy may put your child at risk (2).
- Warfarin, an anticoagulant, is not recommended during pregnancy as it can have adverse effects on the mother and fetus. Studies show that Warfarin can cause fatal bleeding or stillbirth when administered later in pregnancy. It is also associated with adverse neurologic outcomes and low intelligence quotient (IQ) in such children.
- Similarly, thrombolytic therapy can cause premature labor, placental abruption, and fetal demise.
Signs You Should See A Doctor
During pregnancy, swelling and pain in the legs are common. However, if you are worried about your symptoms, consult a doctor.
Additionally, contact your gynecologist if you have any of the following symptoms suggestive of PE (1) (3) (4):
- Sudden unexplained breathing difficulty
- Chest tightness or pain
- Coughing up blood (hemoptysis)
- Feeling unwell or fainting
Diagnosis Of DVT In Pregnancy
Diagnosing DVT in pregnancy can be difficult because the symptoms of DVT are common in pregnancy. However, early diagnosis and appropriate treatment help prevent the maternal mortality associated with DVT.
The steps to diagnose DVT during pregnancy include (2)
- Clinical presentation: Careful risk assessment for the clinical signs of DVT and PE in pregnancy can be helpful, especially for asymptomatic cases (5).
- D-dimer test: A negative D-dimer test and a low clinical suspicion of DVT could help exclude the condition. However, D-dimer values are elevated (positive) even during a healthy pregnancy, making this test non-specific and unreliable for diagnosing DVT.
- Venous compression ultrasonography (VCUS): It is preferred for diagnosing DVT in pregnancy, especially in symptomatic patients. It is non-invasive, safe, and relatively inexpensive. However, VCUS may be unable to locate pelvic vein thrombosis.
- Other imaging studies: If the ultrasound scan is negative and clinical suspicion remains, such in the case of pelvic vein thrombosis, magnetic resonance imaging (MRI) or contrast-enhanced computed tomography (CT) (if MRI is unavailable) could identify DVT. However, since these imaging studies are linked to fetal and maternal radiation exposure, they are not routinely suggested.
Treatment For DVT In Pregnancy
If your doctor suspects DVT, they may refer you to a hematologist or obstetric medicine specialist. The initial line of treatment for DVT is medical treatment.
- Anticoagulant therapy (blood thinners): Injections of low-molecular-weight heparin (LMWH) are administered at the same time every day (or twice daily). The dose varies depending on body weight and is useful for (3)
- Preventing blood clots from growing
- Minimizing the risk of PE or PTS
- Limiting the chances of contracting venous thrombosis again.
However, LMWH should be discontinued at the time of labor and 24 hours before planned cesarean birth. Unfractionated heparin (UFH) can be prescribed instead in the last month of pregnancy as it has a shorter half-life (2).
- Graduated elastic compression stockings: It is an effective adjuvant therapy for improving the pain and swelling of DVT (6).
Inferior vena cava (IVC) filter: It can be used temporarily during pregnancy if you
- Are contraindicated to anticoagulation therapy
- Develop DVT close to the time of delivery (to prevent the risk of PE)
- Contract DVT again despite the anticoagulation treatment
A skilled radiologist usually places IVC filters intravenously as a mechanical barrier to clot dissemination (2) (6).
- Catheter-directed thrombolysis (CDT): This thrombolytic therapy helps reduce bleeding by inserting a multi-side-hole catheter into the thrombus and delivering thrombolytic medicines. It should only be used in cases of life-threatening or limb-threatening maternal thromboembolism. Due to the dangers associated with radiation exposure, this therapy must be avoided in the first trimester (2).
Prevention Of DVT In Pregnancy
If you are at high risk of developing pregnancy-related DVT, the following medications and preventive strategies could help (4):
- Prophylaxis with LMWH is recommended during pregnancy by the American College of Obstetricians and Gynecologists (ACOG) in case of a history of venous thrombosis, thrombophilia, or multiple (more than two) episodes of DVT (2).
- Staying active
- Maintaining a healthy weight
- Wearing prescribed compression stockings to improve blood circulation in the legs
- Frequent leg movement and exercise in case of long hours of travel
Frequently Asked Questions
1. Can a DVT blood clot go away?
In most cases, a DVT blood clot goes unnoticed and disappears. However, if you are diagnosed with this condition, you should take proper treatment to prevent further complications such as pulmonary embolism (7).
2.What not to do with DVT in pregnancy?
Women are more likely to develop DVT during pregnancy, especially those with a history of blood clots (thrombosis), obesity, preeclampsia, or multiple pregnancies. DVT may be life-threatening if it develops into PE, and the treatment mainly involves heparin injections administered subcutaneously. However, staying healthy, active, hydrated, and doing regular leg exercises can help prevent DVT in pregnancy.
Key Pointers
- A swelling in the left lower limb may indicate deep-vein thrombosis (DVT).
- Pregnancy above the age of 35, gestational diabetes, and a few medical conditions may increase the risk of DVT.
- Untreated DVT may cause pulmonary embolism and other post-thrombotic syndromes such as leg ulcers or persistent leg pain.
- Consult your physician if you experience chest tightness, sudden breathing issues, or abnormal heartbeat.
References
- Pregnant? Don\’t Overlook Blood Clots.
https://www.cdc.gov/ncbddd/dvt/features/blood-clots-pregnant-women.html - Devis and M. Grace Knuttinen; (2017); Deep venous thrombosis in pregnancy: incidence
pathogenesis and endovascular management. - Diagnosis and treatment of venous thrombosis in pregnancy and after birth.
https://www.rcog.org.uk/en/patients/patient-leaflets/treatment-of-venous-thrombosis-in-pregnancy-and-after-birth/ - Deep vein thrombosis in pregnancy.
https://www.nhs.uk/pregnancy/related-conditions/complications/deep-vein-thrombosis/ - Venous Thromboembolism Associated With Pregnancy.
https://www.jacc.org/doi/pdf/10.1016/j.jacc.2020.06.090 - Faizan Khan et al.; (2017); Diagnosis and management of deep vein thrombosis in pregnancy.
https://www.researchgate.net/publication/317266064_Diagnosis_and_Management_of_Deep_Vein_Thrombosis_in_Pregnancy - Deep vein thrombosis (DVT): Overview.
https://www.ncbi.nlm.nih.gov/books/NBK425364/ - Preventing Deep Vein Thrombosis.
https://www.acog.org/womens-health/faqs/preventing-deep-vein-thrombosis - DVT (deep vein thrombosis).
https://www.nhs.uk/conditions/deep-vein-thrombosis-dvt/

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.













