Why Do Babies Choke And How To Prevent It?
A baby choking on an object can be dangerous; follow important tips to handle it.

Image: Shutterstock
In This Article
Babies choking on swallowed objects can be the worst nightmare for any parent. Nevertheless, babies may choke on food or too much breast milk as well. It is worse if you cannot understand what has caused the choking. Whatever be the reason, you must be prepared for any such situation rather than losing time in panicking. It is essential to learn how to deal with choking in infants to save lives. Keep reading this post as we explain what you should do if you see a baby choking, how to prevent it, and age-appropriate first aid methods.
Why Do Babies Choke?
Babies, specifically those who move around a little and can grab things, are curious. Their way of exploring the world is through their mouth. Anything interesting or fascinating goes straight into the mouth, regardless of its size, which can eventually lead to choking. More foreign body aspirations occur in children younger than three years than in other age groups, with a peak between the first and second birthdays.
Babies and toddlers have limited control over the expulsion of air, which makes it difficult for them to clear their windpipe with one exhalation. When the child is unable to get something stuck in the windpipe out, they could choke.
What Should You Do If A Baby Is Choking?
Call for emergency medical help and provide first aid in the meantime.
First aid for choking in infants has multiple steps. The techniques may vary, depending on the baby’s age.
Here is what you should do when a baby is choking (1).
i. Babies below one year
Perform the first aid as instructed below, but keep in mind that the infant is delicate and should not get hurt in the process.
Step 1: Check what is causing the blockage
- Find out what the baby is choking on. They can choke on anything including saliva, mucus, small chunks of food or a foreign particle.
- Babies younger than six months are most likely to choke on liquids such as breast milk or formula.
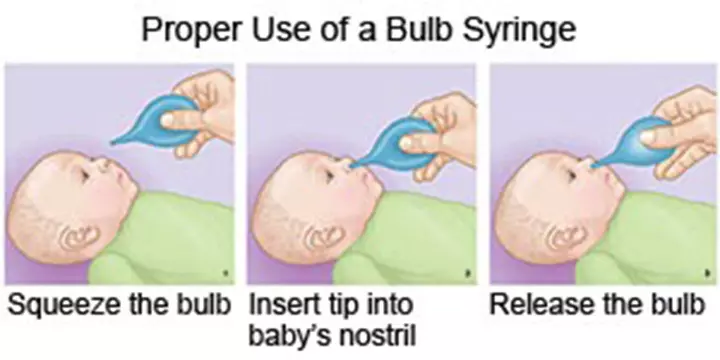
- If you suspect that the choking is due to excess milk or water, and if the child is less then 6 months, use a bulb syringe to remove it. Squeeze the bulb syringe and gently place the tip into the infant’s mouth.
- Slowly release the bulb so that it draws mucus or fluid out of your baby’s mouth, Once the bulb has expanded, remove it from your baby’s mouth. Squeeze the contents onto a tissue.
- Repeat if needed.
- If the baby eats solids, then it may not be possible to remove the obstruction with a bulb syringe. Do not put your finger into the baby’s mouth to remove the lodged item since you could push it deeper within.
- Let the baby cough. Coughing is a natural way of ridding the air pipe of its obstruction.
- Observe if the baby is breathing heavily, has trouble coughing, or is making high-pitched sounds while breathing. It indicates that the choking item is deeply lodged and not easily removable using a bulb syringe or any other mechanism. In that case, you resort to back blows, which is the next step.
Step 2: Back blows
- Sit down on a chair. Place the baby facing downward, on your thigh. Secure the weight of the baby on your left arm and support the baby’s head with your left hand.
- Using the base of your right hand, make firm taps on the baby’s upper back, between the shoulder blades. The tapping should be firm but not too forceful to cause injury. Use enough pressure to dislodge the food item that’s choking the infant.
- Tap about five times, then give a pause to observe if the baby is breathing correctly. If you sense no improvement, then continue the back blows till the food item is dislodged from the windpipe.
Step 3 – Chest thrusts
- If back blows do not help, try chest thrusts. Continue sitting in the same position as you would for the back blows.
- Turn the baby around so that they are facing upwards. The baby’s position should be the same as it was in the back blows technique, except that they are facing upwards.
- Using the index and middle finger, feel for the breastbone of the baby. Once you find it, apply a set of five thrusts on the breastbone.
- Pause for a couple of seconds to see if the baby shows improvement. If not, continue with the sharp chest thrusts.
- The back blows and chest thrusts together are called a modified Heimlich Maneuver (2).
- If the baby is still conscious but appears to be choked, then continue to perform the modified Heimlich Maneuver. However, if the baby shows no signs of improvement and seem unconscious, try resuscitating the baby immediately.
Step 4 – CPR (breathing resuscitation)
- When the dislodging efforts do not work, perform CPR or cardiopulmonary resuscitation (3). CPR is used to revive someone who is unconscious and barely breathing.
- Lay the infant on the back on a flat surface, such as a tabletop or the floor.
- Position the head straight and straighten the legs of the baby. Put your mouth over the baby’s mouth closing it with a seal. Blow out two breaths in two rapid successions. Give a break and repeat it.
Continue with four sets of two blow-outs each (a total of eight times).
- The breath should be powerful enough to make the baby’s chest rise. Watch the baby’s chest fall after it rises. Remember to not breathe out in one go.
- The item stuck in the windpipe may go further down when you blow into the baby’s mouth. However, resuming the infant’s breathing is more important and the object can be removed when the baby resumes breathing and coughs out the obstruction quickly.
Step 5 – CPR (chest compressions)
- If oral resuscitation does not work, then move to the next step.
- Keep the baby in the same position that he/she is during breathing resuscitation. Place your index and middle finger on the breastbone of the baby and perform 30 rapid compressions in one go. Compress enough for the chest to dip 1.5in (4cm).
- Pause for a few seconds before continuing the compressions. Perform no more than 100-120 compressions in a minute (4).
- Tilt the baby’s head back to open the airway and observe if the baby is breathing.
- If the baby still shows no sign of coming back to consciousness, then start CPR again with breathing resuscitation.
Chest compressions often cause the choking item to shift into the mouth from where you can remove it using a bulb syringe. If the item is large, then you may be able to remove it by hand.
ii. Babies older than one year
Step 1: Check what is causing the blockage
- The first step remains the same: removal of the object blocking the windpipe.
- In the case of older infants and toddlers, you may be able to remove the item using your fingers. Do not put your finger deep down.
- If you cannot see the choking item at all, then do not attempt removal. Do not try blind procedure. Move to the next step.
Step 2: Back blows
- The basic procedure is the same as that for babies. However, you can make the toddler stand in a forward-leaning position. It means the toddler leans or tips all the way forward while standing and you support their body with your left arm
- Five firm taps with the base of your hand between the shoulder blades can dislodge the choking item in the windpipe.
Step 3: Abdominal thrusts (Heimlich maneuver)
- You can perform the original Heimlich maneuver on toddlers (infants older than one year) (5).
- Make the toddler stand in front of you. If the toddler is unable to stand, then lift them yourself and get them into a standing position. You can also get the child into a kneeling position, while you kneel right behind them.
- Curl all the fingers of your right hand and make a fist of it. Turn the hand and place the thumb side of the hand little above the belly button of the baby’s stomach. So if you close your fingers to make a fist, the axis between your fingers points towards the belly.
- Keep your hand well below the breastbone and between the ribs. Move your hand a bit to feel if you are not getting in bones in the way.
- Cover the fist with your left palm and perform five firm thrusts in quick successions.
- After five abdominal thrusts, check the condition of the baby. If the baby still displays signs of choking, then continue with the abdominal thrusts maneuver.
Step 4: CPR (breathing resuscitation)
- Make the toddler lie on the back. Position the head and neck straight.
- Cover the mouth of the baby while pinching the baby’s nostrils closed with your index finger and thumb.
- Closing the nose of the infant is the only difference between oral resuscitation performed on babies below one year and those above one.
- Perform a couple of blowouts quickly over a second. Give a pause of a couple of seconds and do it again for about four more times.
Step 5: CPR (chest compressions)
- The baby continues to stay in lying down position on the floor.
- Place the heel of your hand on the breastbone of the baby. Keep the fingers lifted since resting them on the body can cause pressure on the ribs.
- Perform 30 quick successive compressions with the heel of the hand. Compress enough for the chest to sink about 2in (5cm).
- Tilt the baby’s head backward and check if he/she is breathing. Continue with 30 successive thrusts if there is no improvement.
Things To Remember While Giving First Aid:
Here are a few things you should know about choking in babies (6) (7):
- There is no need to perform back blows and chest thrusts when an infant becomes breathless due to asthma, throat inflammation, or injury to the head. In such cases, perform CPR right away.
- If the baby is coughing and choking violently, then let him/her do so for sometime before you start performing back blows and chest thrusts. Coughing is a natural reflex of the body when a person is choked and can help dislodge the item.
- Babies choked with phlegm and mucus should cough it out easily. You can also use a bulb syringe to remove the obstruction from the baby’s throat.
- Do not hesitate to call for help nearby when the baby is choking. There could be a paramedic or a doctor, who can help you deal with the situation better.
The above procedures are first aid methods for immediate help in restoring respiration. Proper treatment will be necessary once the baby is revived. However, there could be scenarios when the baby may not respond to first aid.
What To Do If The Baby Does Not Respond To CPR?
If your baby does not respond to any of the above methods, then wait for the local medical emergency crew to arrive and help. No response to CPR indicates that the problem is severe than it seems and requires the intervention of a medical professional.
How To Prevent Choking In Babies?
Prevention is better than cure or first aid, especially in the case of choking. Here are some tips to prevent your baby/ toddler from choking (8):
- Keep risky food away: Keep small food items such as berries, grapes, small candy, and anything else that is small enough to go into the baby’s mouth and become a choking hazard. Choking can happen due to food items like bread too, which can form blobs inside the baby’s mouth.
- Process food the right way: Finger foods should be no longer than one and a half inches long. When serving food items like meat, you should cut it into much smaller pieces about the size of a baby’s fingernail. Those are easy to swallow without the risk of choking. You must cut the food to a smaller, manageable size when serving it to toddlers.
- Household items can choke too: Your baby can choke on plastic bags, deflated balloons, buttons, and even coins. These items should be stored away from baby’s reach.
- Do not rush the baby while eating: Don’t rush the baby to finish the food, whether it is liquids or solids. If the baby is bottle fed, then choose slow bottle feeding methods such as paced bottle feeding rather than tipping the bottle vertically into the baby’s mouth, which increases the risk of choking.
- Give liquid medicines slowly: A baby can choke on a liquid medicine or even gripe water. So use a spoon or a syringe dropper to give the liquid in a controlled manner.
- Feed a small quantity of food at a time: Offer smaller portions of food instead of spoonfuls in one go, to reduce the chances of choking.
- Make them sit straight while eating: Get your infant and toddler a feeding table so that he/she can sit straight and eat. Sitting straight helps prevent the food from falling into the windpipe and choking. Also, the meal times should be exclusive. No playing or moving around. Do not feed the toddler when they are playing or crawling.
- Teach them to chew: Acquaint toddlers with the need to chew their food properly before swallowing. Make chewing food a part of the good habits regime of the child.
- Never leave babies alone when they are eating: Infants and even toddlers should not be left by themselves during meal time. Sit beside the baby/toddler and stay observant.
- Baby-proof your house: Baby-proof the house once your baby starts crawling around. Store away loose cables and remove small choking hazards from the baby’s reach.
- Place your baby to sleep on his/her back: Sleeping on the back makes it easier for a baby to clear the mucus and liquids in the throat (9).
Frequently Asked Questions
1. At what age do babies choke the most?
Babies younger than five years of age are highly susceptible to choking (6).
2. Are babies likely to choke in their sleep?
Babies have a reflex that causes them to cough up or swallow any liquids they may spit up in their sleep. This reflex ensures they are less likely to choke in their sleep (9).
Knowing why babies choke could help the parents and caregivers be vigilant and avoid such incidents. Babies tend to mouth any object out of curiosity and may accidentally choke themselves. Anatomy of the baby’s airways and their inability to clear foreign objects could increase the risk of choking. You may try to relieve a choking baby with first aid such as back bows and call emergency help. Choking in babies can be avoided by using the proper feeding position, processing foods properly, and keeping objects or toys with choking dangers away from the baby.
References
- How to stop a child from choking
https://www.nhs.uk/conditions/baby/first-aid-and-safety/first-aid/how-to-stop-a-child-from-choking/ - WHAT TO DO IF YOUR CHILD IS CHOKING
https://healthcare.utah.edu/the-scope/kids-zone/all/2014/02/what-do-if-your-child-choking - How to resuscitate a child
https://www.nhs.uk/conditions/baby/first-aid-and-safety/first-aid/how-to-resuscitate-a-child/ - Learn CPR You Can Do It
http://depts.washington.edu/learncpr/infantcpr.html - Choking First Aid Tips
https://www.chp.edu/injury-prevention/common-injuries/choking - Choking Prevention for Children
https://www.health.ny.gov/prevention/injury_prevention/choking_prevention_for_children.htm - Choking – infant under 1 year
https://medlineplus.gov/ency/article/000048.htm - Choking Prevention
https://www.mottchildren.org/posts/your-child/choking-prevention - Myths and Facts About SIDS and Safe Infant Sleep
https://safetosleep.nichd.nih.gov/safesleepbasics/mythsfacts

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Rohit Garoo

















