Graves Disease In Pregnancy: Causes, Symptoms And Treatment
The over-functioning of the thyroid gland leads to theappearance of the symptoms of this condition.
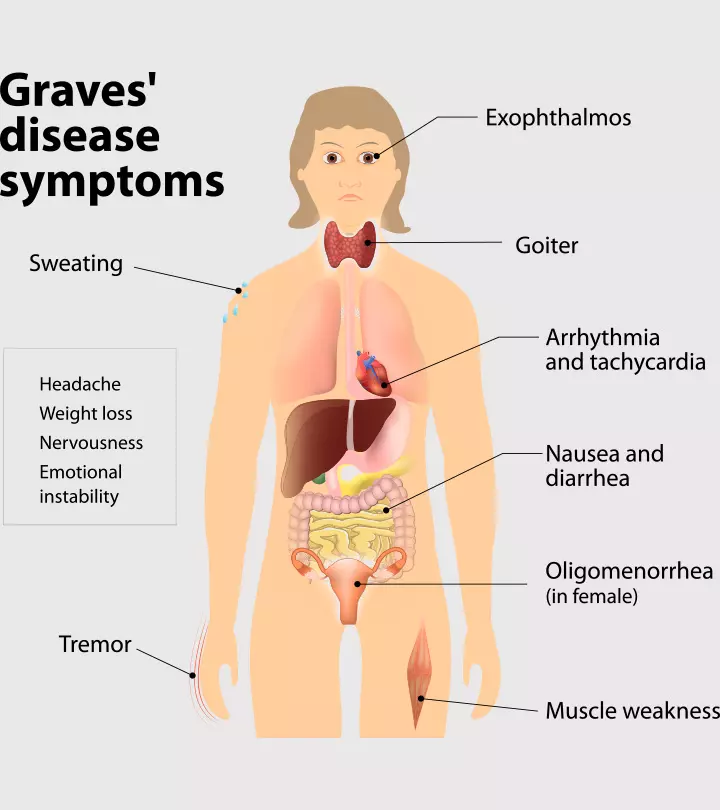
Image: Shutterstock
In This Article
Graves disease is a condition in which the thyroid gland makes excessive thyroid hormone. It is an autoimmune disorder and is a common cause of hyperthyroidism. Graves disease in pregnancy is a common cause of hyperthyroidism. Untreated Graves disease could lead to low birth weight, preterm birth, and preeclampsia complications (1).
This post discusses the causes, risk factors, symptoms, complications, and treatment management for Graves disease in pregnancy.
What Causes Graves’ Disease In Pregnancy?
While most women have a normal functioning thyroid gland during pregnancy, a few have an over-functioning gland. Research suggests that hyperthyroidism during pregnancy occurs when the immune system is triggered to overproduce thyroid-stimulating immunoglobulin (TSI) protein. TSI acts as an antibody and triggers the overproduction of thyroid hormones (2). This overactivity of the thyroid causes the signs and symptoms of Graves’ disease.
What Are The Symptoms Of Graves’ Disease?
The symptoms of Graves’ disease can be easily confused with that of other diseases. Hence, report your symptoms to your doctor for a confirmed diagnosis. The common symptoms include (3)
- Sweating
- Bulging eyes
- Increased heart rate
- Brittle hair
- Frequent bowel movements
- Goiter
- Shaky hands
- Disturbed sleep
- Weight loss
- High blood pressure
Why Is Pregnancy A Risk Factor For Graves’ Disease?
The Endocrine Society recommends that the thyroid hormone levels in pregnant women be maintained at 0.2 to < 0.25mU/L in the first trimester and 0.3–3mU/L in the second and third trimesters (4). However, the hormone levels are always changing during pregnancy, resulting in a higher risk of change in the thyroid hormone levels. This affects the pregnancy and increases the risk of complications such as miscarriage or preterm birth.
How Is Graves’ Disease Diagnosed In Pregnancy?
Graves’ disease is diagnosed in pregnancy with a physical exam of the symptoms and analysis of the patient’s medical history and family history. A blood test is also performed to measure the thyroid hormone level (3). Other diagnosis procedures include a thyroid scan to study the distribution of iodine in the thyroid gland. In Graves’ disease, the iodine spreads throughout the gland, which can be observed in the scan (5).
How Is Graves’ Disease Treated In Pregnancy?
The following methods are used to treat Graves’ disease in pregnancy:
- Antithyroid medication: It is the most sought treatment for Graves’ disease during pregnancy (6). Research suggests that Methimazole (MMI) and Propylthiouracil (PTU) are safe to use during pregnancy (7). PTU is likely to be administered in the first trimester and MMI in the consecutive trimesters.
- Beta-blockers: Their use for the treatment of Graves’ disease is limited (8). They may be used for a few weeks but only under the strict supervision of a medical professional.
- Surgery: Surgery during the first and third trimesters comes with the risk of a spontaneous abortion (9). Therefore, thyroidectomy may be suggested during the second trimester, with an initial dosage of antithyroid medicines only if urgently required.
Does Graves’ Disease Create Complications During Pregnancy?
If left untreated, Graves’ disease might cause the following complications during pregnancy (8) (10):
- Premature birth: The birth of the baby before completing 37 weeks of pregnancy (11).
- Pregnancy-induced hypertension (PIH): It causes high blood pressure, headaches, and blurred vision and usually develops in the second trimester of pregnancy (12).
- Placental abruption: It is a condition where the fetus separates from the uterus, causing sharp pain in the abdomen accompanied by bleeding (13).
- Miscarriage: The loss of the baby in the womb before the 20th week.
Graves’ disease may also give rise to the following birth defects and complications in the fetus:
- Intrauterine growth retardation (IUGR): Poor fetal growth due to high blood pressure or preeclampsia (14)
- Neonatal hyperthyroidism: It is caused by the passage of thyroid-stimulating hormone (TSH) receptor antibodies (TRAb) from the mother through the placenta (15).
Can You Deliver A Baby If You Have Graves’ Disease?
If you undergo proper treatment for hyperthyroidism and follow safety precautions, you can deliver a baby even if you have Graves’ disease.
Frequently Asked Questions
1. Can I pass Graves disease to my baby?
The antibodies that cause hyperthyroidism in Graves disease may pass from the mother to the fetus through the placenta and can affect the baby’s thyroid gland (16).
2. Can I have a healthy pregnancy with hyperthyroidism?
Yes, thyroid problems such as hyper and hypothyroidism if diagnosed and treated on time can enable you to have a healthy pregnancy (17).
3. Does hyperthyroidism make pregnancy high risk?
Uncontrolled hyperthyroidism during pregnancy may pose a high risk to the baby by increasing the possibility of preterm birth and low birth weight, among other complications. It may also pose a threat to the mother by increasing the risk for a fatal form of hyperthyroidism known as thyroid storm (3).
4. Can hyperthyroidism during pregnancy cause autism?
Yes, hyperthyroidism during pregnancy may increase the risk of the development of autism in the baby. Several factors, such as fetal neuronal differentiation from hyperthyroidism and the effect of treatment medications on fetal brain development, may contribute to the cause (18).
5. Can hyperthyroidism cause stillbirth?
The occurrence or presence of high thyroid levels during the later stages of pregnancy or untreated hyperthyroidism may increase the risk of stillbirth (19).
Hyperthyroidism in pregnancy may give rise to complications for the mother and child. However, if proper treatment is provided at the right time, the chances of preterm delivery or low birth weight are significantly reduced. Usually, antithyroid drugs are the first defense against Graves’ disease, but they should only be taken on the advice of a healthcare professional.
Key Pointers
- Graves disease during pregnancy results from hyperthyroidism and commonly displays symptoms such as bulging eyes, palpitations, and brittle hair.
- A complete physical examination, blood tests, and a thyroid scan are some of the ways your doctor will diagnose the condition.
- Beta-blockers, antithyroid medications, and surgery could be suggested based on the severity of the condition.
- Dealy in timely and appropriate treatment may lead to complications.
References
- Graves’ Disease.
https://my.clevelandclinic.org/health/diseases/15244-graves-disease - Graves’ disease.
https://medlineplus.gov/genetics/condition/graves-disease/#causes - Graves’ disease in pregnancy.
https://www.stanfordchildrens.org/en/topic/default?id=graves-disease-in-pregnancy-90-P02460 - Thyroid status and risk of miscarriage.
https://www.thyroid.org/patient-thyroid-information/ct-for-patients/volume-7-issue-12/vol-7-issue-12-p-3/ - Graves’ Disease.
https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease#diagnose - Hyperthyroidism and pregnancy.
https://www.hormone.org/diseases-and-conditions/pregnancy-and-thyroid-disease/hyperthyroidism-and-pregnancy - Fereidoun Azizi and Atieh Amouzegar; (2011); Management of hyperthyroidism during pregnancy and lactation.
https://pubmed.ncbi.nlm.nih.gov/21389085/ - Rashmi Aggarwal and Pradeep Chugh; (2015); Management of hyperthyroidism in pregnancy.
https://www.ijrcog.org/index.php/ijrcog/article/viewFile/486/457 - Yoon-Young Cho et al.; (2005); Management of a pregnant patient with Graves’ disease complicated by Propylthiouracil induced Agranulocytosis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3891081/ - Graves’ disease.
https://www.womenshealth.gov/a-z-topics/graves-disease - Premature birth.
https://www.cdc.gov/maternal-infant-health/preterm-birth/index.html - Preeclampsia.
https://my.clevelandclinic.org/health/diseases/17952-preeclampsia - Placental Abruption.
https://my.clevelandclinic.org/health/diseases/9435-placental-abruption - Intrauterine growth restriction.
https://medlineplus.gov/ency/article/001500.htm - Maria Segni; (2019); Neonatal Hyperthyroidism.
https://www.ncbi.nlm.nih.gov/books/NBK279019/ - Neonatal Grave Disease (Hyperthyroidism).
https://childrensnational.org/visit/conditions-and-treatments/diabetes-hormonal-disorders/neonatal-graves-disease - THYROID CONDITIONS DURING PREGNANCY.
https://www.marchofdimes.org/complications/thyroid-conditions-during-pregnancy.aspx - Mu- Hong Chen et al. (2020); Maternal hyperthyroidism during pregnancy and offspring risks of attention-deficit/hyperactivity disorder and autism spectrum disorder: A nationwide study.
https://www.e-tjp.org/article.asp?issn=1028-3684;year=2020;volume=34;issue=3;spage=115;epage=120;aulast=Chen - Stine Linding Andersen et al. (2014); Spontaneous Abortion Stillbirth and Hyperthyroidism: A Danish Population-Based Study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4224233/#:~:text=Inadequately%20treated%20hyperthyroidism%20in%20earlyan%20increased%20risk%20of%20stillbirth.

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.