Hemolytic Disease Of The Newborn: Causes, Symptoms & Treatment
Fetal ultrasound may reveal symptoms of hemolysis, aiding early treatment.
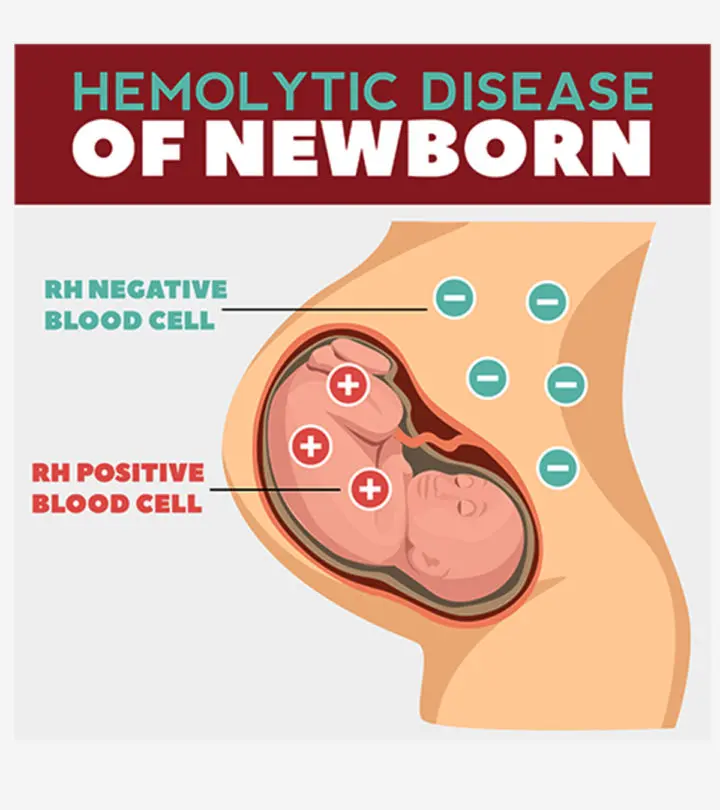
Image: Shutterstock
Hemolytic disease of the newborn (HDN) refers to a blood disorder in newborns that causes the red blood cells (RBCs) to break down faster than usual. The condition is named erythroblastosis fetalis when the baby is in the mother’s womb and HDN once the baby is born.
HDN may lead to several problems and complications, but the condition can be prevented if mothers are administered proper medications during pregnancy.
This post informs you about the causes of HDN and its symptoms, treatment, and prevention.
Causes Of HDN
HDN occurs when the fetus and the mother have different blood groups and Rh factors. The condition most commonly occurs when the baby is Rh-positive while the mother is Rh-negative, irrespective of their blood groups (1).
A small quantity of fetal blood may cross into the mother’s body during natural delivery or during certain events that cause the mixing of maternal and fetal blood. The mother’s immune system detects the Rh antigen and develops Rh antibodies, which are stored in the mother’s body for future use. The mother is now considered Rh-sensitized.
Rh-sensitization is not a concern in the first pregnancy but can be a concern in subsequent pregnancies with an Rh-positive baby. The next time the mother becomes pregnant with an Rh-positive baby, her Rh antibodies actively cross the placenta to destroy the baby’s Rh-positive RBCs, affecting the baby’s health. It leads to a condition called erythroblastosis fetalis, which is called HDN once the baby is born.
Blood group incompatibility may also cause HDN but in milder forms. It leads to less severe problems than Rh incompatibility. It also gets less severe with each subsequent pregnancy.
Risk Factors For HDN
The following events and conditions could directly or indirectly increase the chances of Rh-sensitization, in turn increasing the risk of HDN (2).
- Difference in parent’s blood groups: If the mother is Rh-negative while the father is Rh-positive, the chances of the baby being Rh-positive are higher. This increases the risk of HDN through the increased potential of having a baby with Rh-positive blood.
- Placental abruption: The abnormal detachment of the placenta during pregnancy is called placental abruption. It leads to the mixing of the mother and baby’s blood, making it more likely for the mother to become Rh-sensitized.
- Miscarriage: A miscarriage, especially due to a fall or injury, could rupture the placenta and other tissues, causing mixing of fetal and maternal blood.
- Abortion: It may also cause maternal and fetal blood to combine.
- Prenatal tests: Certain invasive prenatal tests, such as amniocentesis or chorionic villus sampling, require the insertion of a needle into the uterus. This may cause bleeding and subsequent mixing of maternal and fetal bloods, increasing the chances of Rh-sensitization.
Effects Of HDN On Babies
HDN causes rapid destruction of the baby’s RBCs, leading to the following problems in the fetus and newborn (3).
1. Hyperbilirubinemia, jaundice, and kernicterus
The breakdown of the RBCs produces a by-product called bilirubin, which is processed by the liver and excreted in stool and urine. Since HDN causes RBCs to break down quickly, there is more bilirubin in the body than the liver can process. This condition is called hyperbilirubinemia.
Hyperbilirubinemia causes bilirubin accumulation in various tissues, such as the skin and the eyes, causing them to appear yellowish. This condition is called jaundice. If high levels of bilirubin persist and keep on rising, jaundice progresses to kernicterus, which can cause severe neurological damage and seizures in a newborn and may even be fatal.
2. Anemia and hydrops fetalis
HDN leads to the rapid destruction of RBCs, and the bone marrow cannot compensate for it. RBCs contain hemoglobin, which transports oxygen to every cell of the body. Inadequate RBCs and insufficient oxygen supply to various body parts ultimately lead to anemia.
Anemia combined with the quick destruction rate of RBCs affects several organs, especially the liver and spleen, which enlarge than their normal size. In severe cases, the heart may begin to fail, and fluids may accumulate in various organs and tissues. This condition is called hydrops fetalis and is present at birth.
Symptoms Of HDN
The following are the commonly seen signs and symptoms of HDN during the fetal stage and when the baby is born (4).
1. Fetal symptoms
- Ultrasound may show enlarged liver, spleen, or heart. Ultrasound may also reveal some fluid around the fetus’ abdomen, lungs, and scalp, indicating hydrops fetalis.
- If hydrops fetalis is suspected, the doctor may recommend an amniocentesis. It could show yellowish discoloration or the presence of bilirubin in the amniotic fluid.
2. Neonatal symptoms
- A pale appearance of the skin due to anemia.
- A yellow discoloration of skin, eyes, and umbilical cord, suggesting jaundice.
- Babies with hydrops fetalis exhibit swelling across almost the entire body. They also exhibit difficulty in breathing.
- Subsequent tests may reveal enlarged liver and spleen.
Diagnosis Of HDN
The doctor may check for the signs of HDN during pregnancy if the mother is Rh-negative, especially if it is her second or subsequent pregnancy. Tests may also be conducted on the newborn. The following tests could be conducted during pregnancy and after the baby’s birth to diagnose HDN (2).
1. Fetal tests
- Ultrasound scans check for physical signs, such as enlarged organs.
- Amniocentesis checks the presence of bilirubin in the amniotic fluids.
- Fetal blood sampling involves collecting a sample of the baby’s blood from the umbilical cord. The doctor assesses the blood for the presence of Rh antibodies, anemia, and bilirubin levels.
2. Neonatal tests
- Physical examination is done to check for fluid retention in the body and the presence of hydrops fetalis.
- Blood tests to check red blood cell count (for anemia) and bilirubin levels.
- Umbilical cord tests could also be conducted on the detached umbilical cord. Blood from the cord is checked for the presence of Rh antibodies.
Treatment For HDN
The doctor may suggest the following treatment methods depending on the stage of diagnosis of HDN (4).
1. Treatment in the fetal stage
- Intrauterine blood transfusion: A needle with a tube is placed through the uterus to the fetus or the umbilical cord. Fresh donor blood is infused while the baby’s blood with destroyed RBCs and high bilirubin is removed. This procedure may have to be repeated periodically, depending on the improvements shown by the baby in the womb.
- Early delivery: In severe cases, the doctor may suggest an early delivery provided the baby’s lungs are developed. If the lungs are yet to mature, the doctor may administer the mother corticosteroids to help the baby’s lungs mature faster. Early delivery could prevent erythroblastosis fetalis or HDN from worsening.
2. Treatment in neonates
- Blood transfusions: The baby’s blood will be exchanged with donor blood to reduce the effects of anemia and hyperbilirubinemia. It could improve the symptoms gradually.
- Phototherapy: The baby is laid bare skin in an incubator with a special light, which increases the rate of bilirubin’s decomposition. It makes it easier for the body to process and excrete bilirubin. Phototherapy targets hyperbilirubinemia and jaundice effects of HDN.
- Intravenous immunoglobulin: The baby is administered an intravenous immunoglobulin (IVIG) solution made of blood plasma. This helps strengthen the baby’s immune system, reducing the breakdown of RBCs and the effects of hyperbilirubinemia.
Besides the treatment, the baby is also provided other support, such as intravenous nutrition and ventilation (oxygen support), to help the body deal with HDN’s symptoms better.
Prevention Of HDN
HDN due to Rh incompatibility is preventable. Rh-negative mothers who have not been Rh-sensitized can receive injectable Rh immunoglobulin, also called RhoGAM, around the 28th week of pregnancy. It prevents the maternal Rh antibodies from reacting with the baby’s Rh-positive blood. A second shot is needed within 72 hours of delivery, but only if the baby is Rh-positive.
Frequently Asked Questions
1. Do babies survive hemolytic disease?
Yes, babies with hemolytic disease do survive if the problem is diagnosed and treated early. Additionally, the fatal outcomes of the conditions have been considerably reduced due to appropriate use of immunoprophylaxis (measures taken before childbirth) (5).
2. Is hemolytic disease of the newborn curable?
With prompt and proper medical care, complications are rare in hemolytic disease. However, high bilirubin levels, if left untreated, may lead to hearing problems and brain damage. Severe untreated anemia may result in heart failure (6).
Hemolytic disease adversely affects the fetus and the baby. It destroys the baby’s RBC, leading to jaundice and anemia. Depending on the severity, doctors may treat HDN with intrauterine blood transfusion, phototherapy, or other treatment strategies. However, HDN can also be prevented when a medication is injected into mothers who have not been Rh-sensitized. Therefore, if you are unsure of your Rh factor or blood group, it is advisable to get yourself tested before planning your pregnancy to avoid the risk of HDN.
Key Pointers
- Administering proper medications during pregnancy can prevent HDN in mothers.
- HDN causes rapid destruction of the baby’s RBCs, leading to various problems in the fetus and newborn.
- Effects of HDN on babies include hyperbilirubinemia, jaundice, anemia, and hydrops fetalis.
References
2. Hemolytic Disease of the Newborn (HDN); University of Rochester Medical Center
3. Andrew W. Walter, Hemolytic Disease of the Newborn; MSD Manuals
4. Hemolytic Disease of the Newborn; Children’s Hospital Of Philadelphia
5. Victoria Hall and Indirapriya Darshini Avulakunta; Hemolytic Diseases Of The Newborn; NCBI (2025).
6. What is Hemolytic Disease of the Fetus and Newborn (HDFN)?; Nationwide Children’s Hospital
Read full bio of Dr. Prakhar Nyati