High Cholesterol In Pregnancy: Types, Symptoms And Treatment
Elevated cholesterol levels in pregnancy are linked to preeclampsia and preterm birth.
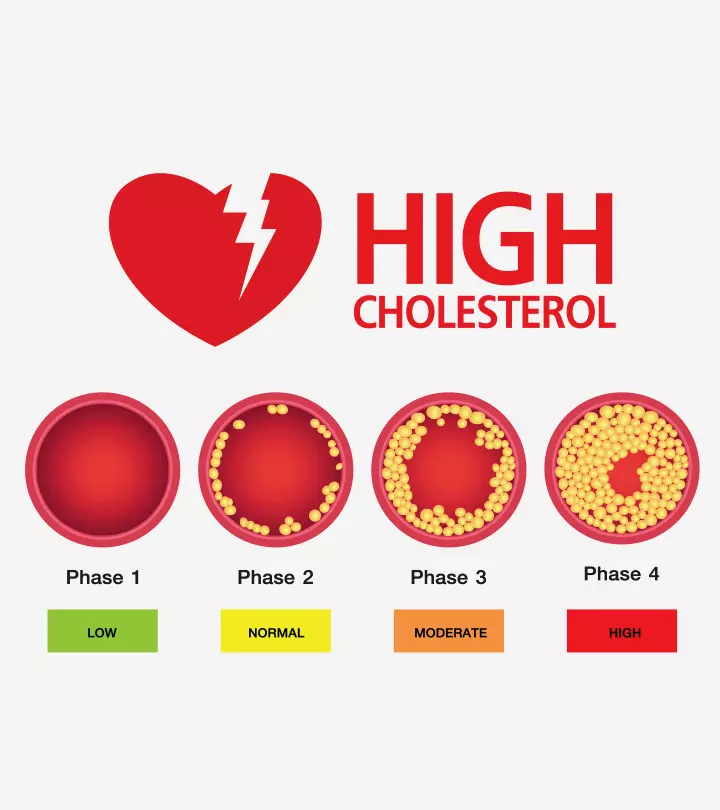
Image: Shutterstock
In This Article
The desirable level of total cholesterol for adults is less than 200mg/dL. However, it is natural to have high cholesterol in pregnancy, which helps support the healthy development of the fetus. Cholesterol is a waxy substance produced by the liver to aid in several functions, such as hormone synthesis. Full-fat dairy and poultry help the body obtain the necessary amount of cholesterol (1) (2) (3).
An increase in cholesterol levels during pregnancy is temporary and does not cause any adverse effects on maternal or fetal health. However, for women with high triglycerides before pregnancy, the cholesterol levels can increase further and have adverse effects.
Read about the risks and tips to control high cholesterol during pregnancy.
Different Types Of Cholesterol
Cholesterol has two types, namely LDL (low-density lipoprotein) and HDL (high-density lipoprotein) cholesterol (4) (5). There are also triglycerides (TGs) found in the bloodstream.
- LDL cholesterol makes up most of the body’s cholesterol, the excess of which is linked to an increased risk of cardiovascular disease and stroke. It’s the reason that LDL cholesterol is also known as “bad cholesterol.”
- HDL cholesterol is known as the “good cholesterol” because it captures the bad cholesterol and takes it away from the arteries.
- Triglycerides are not cholesterol but fat in the bloodstream that comes from the extra calories you get from the food. Your body stores TGs in the fat cells and releases them when you need energy. If you have high triglyceride levels, they raise your risk of cardiovascular diseases.
Signs And Symptoms Of High Cholesterol During Pregnancy
There are no specific signs and symptoms of high cholesterol levels during pregnancy. Hence, unless a blood test is done, high cholesterol levels can go undetected for years. In such cases, the extra cholesterol can deposit in the artery walls, leading to plaque formation. Continuous plaque build-up can narrow the arteries and lead to a blockage.
A blocked artery to the heart could cause a heart attack. If the blockage is in the artery to your brain, it could cause a stroke. Thus, monitoring blood cholesterol levels before and after pregnancy is crucial, especially if you have familial hypercholesterolemia (FH). Familial hypercholesterolemia (FH) is a genetic disorder that causes an individual’s LDL cholesterol levels to increase, raising their risk of coronary heart diseases from a young age (6).
Diagnosis Of High Cholesterol Levels During Pregnancy
A lipid profile or lipid panel test is a blood test that can help diagnose hypercholesterolemia. Most healthy pregnant women don’t need to monitor their cholesterol levels during pregnancy. However, if a woman has risk factors for cardiovascular diseases, the doctor may order a lipid profile test.
The test will evaluate the total cholesterol, LDL, and triglycerides levels in the blood. The latest cholesterol guidelines advise keeping the cholesterol levels within the following limits (7).
1. Total cholesterol (mg/dL)
- Less than 200: Desirable
- 200 to 239: Borderline high
- 240 or more: High
2. LDL cholesterol (mg/dL)
- Less than 100: Optimal
- 100 to 129: Near-optimal
- 130 to 159: Borderline high
- 160 to 189: High
- 190 or more Very high
3. Triglycerides (mg/dL)
- Less than 150: Normal
- 150 to 199: Borderline high
- 200 to 499: High
- 500 or more: Very high
According to experts, cholesterol levels increase during pregnancy by 25 to 50 percent (8). This rise is crucial for the production and function of steroid hormones (estrogen and progesterone), which are responsible for the smooth transition of pregnancy and proper development of the baby (3). Cholesterol has a role in fetus brain, limb and cellular development as well as, in healthy breast milk.
Possible Effects Of High Cholesterol On The Baby
High cholesterol levels during pregnancy seldom harm the fetus. However, if your cholesterol (LDL cholesterol) levels rise too high, they may cause the following effects (9).
- Pregnancy-induced hypertension
- Preeclampsia (toxemia of pregnancy)
- Gestational diabetes
- Preterm delivery and development of atherosclerosis in offspring
Treatment For High Cholesterol During Pregnancy
Cholesterol-lowering drug use in the first trimester of pregnancy is associated with an increased risk of pregnancy loss (10). Hence, experts advise against using cholesterol-lowering medications, such as statins and ezetimibe, three months before you try conceiving, during pregnancy, and until breastfeeding as they are connected with abnormalities in babies. Bile acid sequestrants are cholesterol-lowering drugs that don’t cross the placenta and affect the baby, but increase mothers gastrointestinal problems. Hence, their use during pregnancy under expert guidance could be considered.
Typically, cholesterol levels return to normal three months after childbirth. However, if you have a history of hypercholesterolemia or have risk factors for cardiovascular disease, your healthcare provider will likely test your cholesterol levels after childbirth. Then, if needed, they will prescribe you cholesterol medications once your baby is weaned off.
Natural Ways To Manage Cholesterol Levels During Pregnancy
The best way to manage your cholesterol levels during pregnancy is to keep them under control right from the start. You may consider the following measures to achieve healthy cholesterol levels.
- Consult a nutritionist and get a personalized low-fat diet plan.
- Eat a well-balanced, healthy diet containing various low-fat foods, such as low-fat dairy and lean meat.
- Include more fiber-rich foods, such as whole grains, seeds, legumes, and fresh fruits and veggies, in your diet.
- Monitor your weight and keep strict control on your total and saturated fat content.
- Stay physically active and indulge in at least 30 minutes of pregnancy-safe exercises, such as walking or swimming, daily.
- Avoid eating fried and highly processed foods, such as cakes, pastries, and biscuits.
- Abstain from high saturated fat foods, such as red meat, butter, ghee, and margarine.
- Stay stress-free and indulge in mindful activities, such as deep breathing exercises and meditation for a healthy pregnancy.
Besides these, talk to your healthcare provider about omega-3 supplementation. According to the American Heart Association (AHA), consuming prescribed omega-3 supplements can lower your chances of developing heart issues (11).
Frequently Asked Questions
1. When does cholesterol increase during pregnancy?
Research states that, in most women, there could be an elevation in mean cholesterol levels from the first trimester. These levels may rise in the subsequent months of pregnancy and fall swiftly post delivery (9).
2. Can high cholesterol cause congenital anomalies?
Limited evidence exists to prove an association between cholesterol levels and congenital anomalies. However, one study revealed that factors such as a history of obesity, diabetes, and abnormal maternal folate status could increase the risk of adverse pregnancy outcomes, such as congenital disabilities (12).
Cholesterol is a fatty substance that naturally rises during pregnancy due to physiological changes. These changes are essential for the healthy development of the baby and the smooth progression of pregnancy. For most healthy expecting moms, this rise doesn’t cause any concerns. However, if you had high cholesterol pre-pregnancy or risk factors of cardiovascular diseases, keeping your cholesterol levels within healthy limits can help avert adverse pregnancy outcomes.
Key Pointers
- Increased cholesterol levels are not uncommon during pregnancy but may put mother and fetus at risk of adverse outcomes.
- It is vital to monitor cholesterol levels in pregnancy, especially if you had high triglycerides before pregnancy or have a family history of hypercholesterolemia.
- High cholesterol during pregnancy increases your risk of heart diseases, hypertension, diabetes, and preterm labor.
- Cholesterol-lowering drugs are not advised (unless necessary) during pregnancy.
- Therefore, you may follow home care tips, including a low-fat, fiber-rich diet, indulging in safe and mild physical activities, avoiding deep-fried and fatty foods, and practicing pregnancy yoga to manage cholesterol levels while pregnant.
References
- Cholesterol.
https://medlineplus.gov/cholesterol.html - Cholesterol Levels.
https://medlineplus.gov/lab-tests/cholesterol-levels/ - Pregnancy and blood fats.
https://www.heartuk.org.uk/cholesterol/pregnancy-and-blood-fats - LDL and HDL Cholesterol: “Bad” and “Good” Cholesterol.
https://www.cdc.gov/cholesterol/ldl_hdl.htm - What Your Cholesterol Levels Mean.
https://www.heart.org/en/health-topics/cholesterol/about-cholesterol/what-your-cholesterol-levels-mean - Familial Hypercholesterolemia.
https://www.cdc.gov/genomics/disease/fh/FH.htm - Kim K. Birtcher and Christie M. Ballantyne; (2004); Measurement of Cholesterol.
https://www.ahajournals.org/doi/full/10.1161/01.cir.0000141564.89465.4e - Women with FH & Pregnancy.
https://thefhfoundation.org/familial-hypercholesterolemia/women-with-fh-pregnancy - Änne Bartels and KeelinO’Donoghue (2011), Cholesterol in pregnancy: a review of knowns and unknowns.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4989641/ - Pregnancy, statins, and high cholesterol: What women need to know.
https://utswmed.org/medblog/statins-pregnancy-familial-hypocholesteremia/ - Prescription omega-3 medications work for high triglycerides, the advisory says.
https://www.heart.org/en/news/2019/08/19/prescription-omega3-medications-work-for-high-triglycerides-advisory-says - Adolfo Correa and Jessica Marcinkevage; (2013); Prepregnancy obesity and the risk of birth defects: an update.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5866281/#!po=50.0000

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.