Birth Control While Breastfeeding: 11 Best Methods For New Moms
Explore safe, effective ways to prevent pregnancy without affecting your nursing routine.

Image: Shutterstock
You are breastfeeding and all busy taking care of your little one. That does not stop you from bonding with your partner. But the worry of another pregnancy is always on your mind. So what is the way out?
Enter contraceptives. There are various contraceptives, but which one should you choose while breastfeeding? Keep reading as MomJunction tells you about contraception during breastfeeding and the best way to avoid pregnancy.
Can You Choose Birth Control While Breastfeeding?
Yes. If you have a breastfeeding infant to care for and do not want another child anytime soon, you should go for birth control.
Doesn’t Breastfeeding Work As A Contraceptive?
Yes, but it is subject to specific conditions. Breastfeeding leads to the secretion of hormones called prolactin and oxytocin. These hormones prevent the secretion of the ovum (egg) by the ovaries, eventually preventing pregnancy (1). However, this happens only in some cases (2):
- It works as a contraceptive only during the first six months of breastfeeding.
- There should be no periods, which means you are not ovulating yet.
- The baby should be exclusively breastfed, i.e., 85% of the baby’s feeds should be breast milk.
Only if the above conditions are met can you rely on breastfeeding for birth control. This method of birth control is called lactational amenorrhoea method.
Lactational amenorrhoea method is the cheapest and the best way to prevent pregnancy while breastfeeding. But it may not work once the baby is over six months of age or you are ovulating again. In such cases, you should also use alternative birth control measures.
[ Read: Menstruation During Breastfeeding ]
What Are The Various Birth Control Options While Breastfeeding?
There are several contraceptives to prevent pregnancy. A birth control measure can be categorized into two: hormonal birth control and non-hormonal birth control methods.
Hormonal birth control methods
These methods influence the hormonal functions of the woman’s body to prevent conception. Birth control is achieved through modification of hormonal secretions that govern the release of an ovum (egg) by the ovaries. Popular hormonal birth control methods include:
1. Birth-control pills
- Also called “The Pill,” it is the first thing that most women reach out to when they want to avoid pregnancy. Oral birth-control pills contain the hormones estrogen and progestin that work together to prevent ovulation (3).
- The pill also modifies the uterine lining and the mucus in the cervix to prevent sperms from reaching farther.
- Birth-control pills are available in packs of 21, 28, and 91 tablets. The packet comes with the instructions of dosage, which is one tablet taken every day with food or milk.
- Once you complete a course, you may have to wait a week or so before starting another pack, depending on the manufacturer or gynecologist’s instructions.
- The duration of use depends on your requirements or the doctor’s instructions.
- If your baby is younger than six months and exclusively breastfed, then you can start using birth-control pills only when you resume your periods. The course of medication begins on the fifth day of your period.
- The birth control pill can have side effects such as a headache, mood swings, skin problems, heavy discharge of blood during periods, etc. These effects vary among different women and tend to be present during the first three months of pill consumption. The effects usually taper away as the body adjusts to the regular intake of the pill hormones (4).
2. Progestin-only pill
- These birth-control pills contain only the progestin hormone (5).
- The dosage is similar to that of the ‘pill’.
- Progestin pills are often considered safer for breastfeeding mothers because they only alter one hormone. However, both pills are said to diminish the milk supply a little (6).
- You can prefer a progestin-only pill to avoid estrogen, which could affect your milk supply. Progestin is safe and usually does not affect the infant’s health.
[ Read: Period After Breastfeeding ]
3. Medroxyprogesterone injection
- Medroxyprogesterone is a compound that prevents ovulation and also thins the lining of the uterus (7).
- The compound is taken through an injection administered intramuscularly (injected into the muscle) or subcutaneously (injected under the skin). You need to visit the doctor’s clinic for the shots.
- Intramuscular shots need to be taken once in 13 weeks while subcutaneous shots are required once in 12-14 weeks. The doctor may recommend another schedule depending on the dosage given.
- Unlike contraceptive pills, Medroxyprogesterone does not impact breast milk production. But the compound causes the most severe side effect on the woman’s health by reducing bone density.
- Medroxyprogesterone reduces the calcium and mineral reserves in the bones causing the bone to become weak (8). Minerals may not return to normal even after discontinuation of the medicines, thus increasing susceptibility to osteoporosis in the long run.
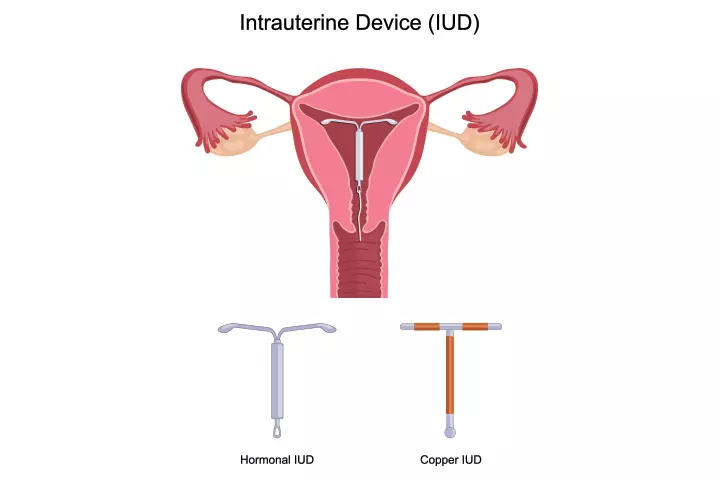
4. Hormonal intrauterine device (IUD)
- Hormonal IUD is a T-shaped sterile, flexible plastic device inserted into the uterus (9).
- Insertion and removal are done through the vagina, which means you do not have to undergo surgery.
- The hormonal IUD contains a hollow central tube that contains a hormone, like progestin, which is gradually secreted into the uterus to prevent ovulation.
- Hormonal IUDs achieve birth control by stopping ovulation, altering the cervix lining, and thickening the mucus to prevent the sperms from moving.
- IUDs (both hormonal and non-hormonal) are more than 99% efficient in preventing pregnancy.
- A hormonal IUD can last three to five years after insertion. It is also reversible, which means once you are ready to conceive, the doctor can remove the device to restore fertility.
- Downsides are that it can cause cramps and backache sometimes, although the frequency and intensity of pain decrease over time. Hormonal IUDs also have to be checked by a doctor once in a while.
5. Contraceptive vaginal ring
- The contraceptive vaginal ring is a tiny hollow tube inserted into the vagina (10). The hollow tube contains the hormone progestin and sometimes even estrogen.
- When placed into the vagina, the ring releases the hormone into the cervix to prevent ovulation.
- Its functioning is similar to that of an IUD.
- You can insert the ring yourself, but doctor consultation is essential before you do.
[ Read: Antibiotics While Breastfeeding]]
6. Progestin arm implant
- The progestin-only implant is the size of a toothpick inserted under the skin, usually in the upper arm (11).
- It works the same way as the other progestin-based contraceptives, but it releases the hormone directly into the bloodstream.
- The implant is 99.95% effective in preventing pregnancy.
- On the flip side, implanting the device requires a surgical procedure, which means you need to stay in the hospital for a day or two. You may also need to have post-surgery antibiotics, which could pass into the breast milk.
7. Birth control skin patch
- The birth control skin patch is small, square-shaped, paper-like sticker that contains the hormones progestin and estrogen.
- The patch can be stuck on the upper arm, abdomen, buttocks, or back. Hormones are gradually absorbed into the skin from where they enter the bloodstream and reach the ovaries and uterus, where they prevent ovulation and also thicken the cervix lining.
- Skin patches are easy to use, but can only be purchased through a doctor’s prescription (12). Patches should be used only when you have resumed your periods. You may require multiple patches for different weeks of the period.
Non-hormonal birth control methods
These methods do not alter the hormonal secretion of the body. Non-hormonal birth control methods either work as a physical barrier or surgically change the anatomy of the body to prevent conceiving.
8. Condoms
- Condoms are available for both men and women.
- A condom is the simplest and perhaps the safest (no side effects) birth control method while breastfeeding. Condoms work as a physical barrier between sperm cells and the cervix by covering the genitals. Thus preventing pregnancy.
- Condoms are made of several materials, but latex is by far the most common. Those allergic to latex can use condoms made of polyurethane, which is a type of plastic.
- Male condoms have 82% success rate while female condoms have a success rate of 79% (13) (14). However, they are inexpensive when compared to other contraceptive methods. Condoms are also readily available and do not require doctor consultation.
9. Diaphragm and cervical cap
- These are soft, cup-shaped barriers inserted into the vagina to fix over the cervix and close its opening.
- The diaphragm cup and the cervical cap work the same way, by covering the opening to the cervix and preventing the entry of sperms. The diaphragm cap is made from rubber while the cervical cap is made from silicone or latex. The cervical cap is not commonly used or available in some countries such as the US (15).
- The cup/diaphragm can last up to two years and do not alter the hormone levels in the body.
- A diaphragm has a success rate of 84%. The cervical cap has a success rate of only 60% for women who gave birth at least once.
- These are less readily available birth control methods than condoms and are much more difficult to use.
[ Read: Painkillers While Breastfeeding]
10. Tubal sterilization
- It is a surgical method where the fallopian tubes that carry the ovum (egg) from the ovary to the uterus are clamped or split. If split, then the ends are clamped (16).
- Tubal sterilization is called tubal ligation or tubectomy.
- It is a permanent birth control procedure performed by a surgeon. The procedure involves using anesthesia, which could pass into the breast milk and affect the health of the baby.
11. Non-hormonal IUD
- It is the same as a hormonal IUD, except it does not contain hormones.
- A non-hormonal IUD releases copper into the uterus and interferes with the implantation of the ovum in the uterus, thus preventing pregnancy (17).
- The only downside is that it has to be regularly checked by the user and the doctor in case of problems.
With so many options on the table, picking one can be difficult unless you know the advantages and disadvantages of each.
Which Birth Control Method Is The Best?
Both hormonal and non-hormonal methods have their pros and cons.
Hormonal birth control
| Pros | Cons |
| Has a very high success rate | May have side effects |
| Works well in the long-term, sometimes for years together | Compounds can pass into milk |
| You can choose from multiple methods | Requires doctor consultation |
| May cause long-term health problems like cancer (18) |
Non-hormonal birth control
| Pros | Cons |
| Does not affect breast milk production or quality | Low success rate, high rate of failure |
| Will not affect the health of the baby | Limited options |
| Easy availability of most methods | The tubal sterilization method is irreversible |
| Can be less expensive compared to hormonal methods |
Each method has its advantages and disadvantages. What’s best for you entirely depends on what works for you and your partner and how it affects your long-term plans. If your objective is birth control and prevention of sexually transmitted diseases (STDs), then non-hormonal, physical barrier methods like condoms are the best. But if you are looking for highly efficient birth control methods, then a hormonal method should be good enough.
[ Read: Marijuana While Breastfeeding ]
If you do not want to have any more kids, then permanent birth control methods such as the tubal ligation are ideal. In any case, discuss your choice with your partner, and healthcare provider with due consideration of yours and your baby’s health. Your doctor can help you pick the right method depending on your preferences and the baby’s age.
What is your preferred choice of birth control during breastfeeding? Tell us about it in the comments section.
Read full bio of Rohit Garoo