Keto For Kids: Its Safety, Possible Uses And Side Effects
Design an effective and safe keto meal plan for your child.
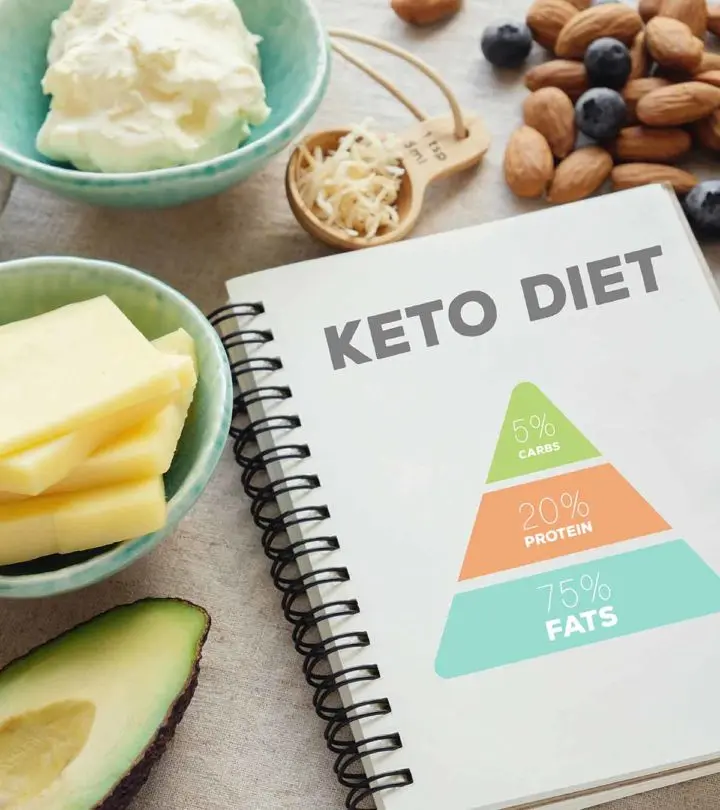
Image: Shutterstock
In This Article
As the ketogenic or keto diet has gained popularity as a fad diet and trendy weight-loss plan, it has attracted a growing number of older children and teenagers seeking weight-loss options. But is keto for kids and teens considered safe?
The keto diet is a specific eating plan that consists of a low-carbohydrate, moderate-protein, and high-fat intake (1). The diet was first used to treat intractable epilepsy in the 1920s, and later, it was also recommended for people with other health issues, including diabetes and cancer.
Read this post to know more about the ketogenic diet for kids and teens and its potential uses, side effects, and more.
How Does Ketogenic Diet Work?
A ketogenic diet is a form of a low-carbohydrate diet where most calories come from fat. Carbohydrate intake is reduced to as low as 20 to 50 grams per day (2), while dietary fat is increased by about four grams of fat consumed for every gram of carbohydrate and protein. Thus, almost 90% of calories in a ketogenic diet come from fat (3).
The name ketogenic means producing ketones. The diet mimics fasting since the body has inadequate glucose, the primary source of energy derived from carbohydrates. Therefore, the body enters ketosis, a state where it uses fat to synthesize ketones, the compounds which become the primary source of energy for the body (4).
The use of ketones for energy alters the body’s metabolism and leads to changes, such as a decrease in insulin levels and fat storage. Some other changes that can be noticed include a reduction in seizures, body weight, and blood sugar. Ketones can be detected in urine, blood and breath.
Is Keto Diet Safe For Children And Teens?
The keto diet is safe for children and teens when prescribed by a doctor for medical reasons and tailored by a dietician. A normal, healthy child/teen needs about 130 grams of carbohydrates per day through foods from different food groups (5). However, in the keto diet, carbohydrate intake is reduced to approximately 10-20% of the total calorie intake. Thus, it requires careful measurement of calories, fluids and proteins and weighing of food portions.
Foods rich in carbohydrates are also sources of other essential nutrients. Therefore, a keto diet not supervised by a doctor may increase the risk of nutritional deficiencies in children.
Discuss the diet with your doctor first before using it to control your child’s epilepsy. For ketosis, the diet typically starts in an in-patient setup where the child’s diet is changed gradually under strict monitoring. It ensures that the child adjusts to their new diet safely, and meanwhile, the families also carefully understand the dietary requirements (6).
What Are The Uses Of The Keto Diet For Children?
Keto diet for children is primarily used for the treatment of epilepsy since the diet has been scientifically proven effective against this condition (7) (8). The diet may be used in conjunction with medicines or used as primary treatment, like in cases of refractory epilepsy, a severe form of epilepsy where seizures cannot be managed with antiepileptic drugs (9).
The following are some salient points about the use of keto diet to treat epilepsy in children.
- In cases of refractory epilepsy, a ketogenic diet can be a more effective treatment option than administering a new medication (3).
- Ketogenic diet could be considered when antiepileptic drugs have side effects that outweigh the benefits.
- Children with epilepsy may display a reduction in the frequency of seizures while on a ketogenic diet (10).
- Research shows that about two-thirds of children following a ketogenic diet have more than 50% reduction in seizures (6). About 25% of these children have a chance of becoming seizure-free.
- If the child shows signs of improvement due to a keto diet, then the doctor may reduce antiepileptic medications, thus minimizing the side effects experienced by the child.
- According to the American Academy of Pediatrics (AAP), several epilepsy syndromes, like Dravet syndrome, Doose syndrome, Rett syndrome, GLUT-1 (glucose transporter type-1) deficiency, and tuberous sclerosis complex, often respond positively to a ketogenic diet (7) (11).
Furthermore, several clinical studies support using the keto diet as a subsidiary cancer therapy ((12). However, targeted studies are needed to validate the recommendation.
It is not known if a keto diet for children is helpful beyond treating epilepsy. There is no long-term research analyzing the effects of the diet on conditions such as overweight and type 2 diabetes (8). If your child does not have epilepsy and you want them to try the diet for weight loss or other reasons, then consult a pediatrician first.
For How Long Can Children Follow Ketogenic Diet?
The recommended duration for adherence to keto diet varies as per the case of epilepsy. If the diet shows effectiveness, then the doctor may recommend discontinuing the diet after two years of seizure control (6). Children and teens with fewer changes in their condition may have to continue the diet for several years.
In some cases, with improvement, the use of a modified Atkins diet may be allowed.Modified Atkins diet is a less restrictive variation of the ketogenic diet with flexible nutrient intake.
What Are The Possible Side Effects Of Keto Diet?
Some of the common side effects that you may observe in children and teens following the keto diet are (11) (13) ((14):
- Dehydration
- Gastrointestinal issues, like nausea/vomiting, diarrhea, or constipation
- Fat intolerance and gastritis
- Electrolyte imbalance and acidosis
- Mood changes, hyperactivity, and irritability
- Micronutrient deficiencies, such as iron-deficiency anemia
Some severe side effects of keto diet may include:
- High cholesterol
- Hypoglycemia (low blood sugar)
- Kidney stones
- Poor bone health
Some of the side effects, like dehydration, can be managed by monitoring the hydration levels of children and teens, while some others, like mood changes, may subside with time and adjustment with the diet.
Doctors can reduce the side effects through an appropriate adjustment to the diet and supplementation. Most commonly calcium, vitamins D, B complex and selenium need to be supplemented. Following the keto diet under strict pediatric guidance could minimize the overall risk of any adverse effects. Also it is important that the growth (weight and height) of children on this diet are monitored at regular intervals.
How To Help A Child Follow The Keto Diet?
Keto diet involves several dietary restrictions that can be difficult for children and teens to manage. Therefore, parental involvement plays an essential role.
Parents can take some steps to help their child/teen adjust to their new diet with ease (13).
- Divide the daily meal plan into three meals and two snacks. Each meal should have a small portion size as the food is high-fat.
- Restrict eating any other foods outside the meal plan.
- Keep all the foods that your child is restricted to eat away from their reach, and provide them with healthy, keto-friendly snack options.
- Avoid eating carbohydrate-rich foods, like potato chips, bread, rice, and pasta, in front of your child/teen, as it may lead to cravings.
- Maintain regular follow-ups with the doctor and dietitian/nutritionist, and discuss your child’s dietary issues.
- Prepare meals that look tempting and colorful. It motivates children/teens to eat happily. Look for keto-friendly foods options to maintain variety while keeping the carbohydrate intake low.
- Ensure family support to a child for keeping them motivated to follow the diet.
- Young children going to kindergarten, school, or social events should carry their meals with them.
- Teachers, educators, and caregivers must be informed about your child’s special dietary requirements to avoid ingestion of food outside the meal plan.
Frequently Asked Questions
1. At what age can you start keto for children?
Keto diet may be tried in children between the ages of one and twelve years who have seizures that do not respond to conventional treatments or have certain disorders, such as glucose transporter or pyruvate dehydrogenase deficiencies (15).
2. How do I transition my child to keto?
Ketogenic diet is prescribed for children with certain conditions, and not as a weight loss plan. If your child has a condition and the doctor has prescribed the keto diet, it may be started at the hospital (may require four to five days of hospital stay) or at home. During the admission, children will be given a ketogenic formula drink 48 hours before moving on to special ketogenic meals. Close monitoring of blood ketones and blood glucose levels will occur.
At home it takes about two weeks to get to the target keto diet (required tests should be done in the hospital first). During home initiation, food is started from day one. The food needs to be weighed. The diet may not be nutritionally balanced, and your child may need vitamin and mineral supplements. The dietitian will guide you with all the procedures (16).
Keto for kids is safe when a doctor recommends it to manage conditions such as epilepsy and is done under the supervision of a dietician. Children are growing in age and activity, and they require carbohydrates to meet their energy needs and nutrients. A Keto diet for children is also recommended to manage epilepsy and medical therapy. Dehydration, nutritional deficiencies, and gastrointestinal issues are common with ketogenic diets. A pediatric dietician helps plan a keto diet with micronutrient supplements and other healthy foods to avoid negative effects.
Infographic: Alternatives To Keto Diet For Pediatric Epilepsy
Several non-drug interventions may be effective in controlling the symptoms of epilepsy in children. They may also help support any drug therapy by reducing the number and dosage of medications required, resulting in reduced side effects. Check out this infographic to learn about dietary interventions other than keto and neurostimulation therapy for epilepsy.
![non drug interventions for pediatric epilepsy [infographic]](https://cdn2.thebridalbox.com/wp-content/uploads/2020/08/Non-Drug-Interventions-For-Pediatric-Epilepsy.jpg.webp)
Key Pointers
- A keto diet is deficient in carbohydrates, with 90% of its calories coming from fat.
- A ketogenic diet is safe for children only if the reason is medical and suggested by a doctor.
- Look out for side effects such as dehydration, gastrointestinal disturbances, acidosis, or mood changes and discuss with your doctor for adjustments.
References
2. Low Carbohydrate Diet; NCBI
3. Ketogenic Diet: Treating Children’s Seizures with Food; Healthy Children; American Academy of Pediatrics
4. Ketogenic Diet; NCBI
5. Joanne Slavin and Justin Carlson; Carbohydrates; NCBI6. Ketogenic Diet for Kids; Children’s Hospital of Philadelphia
7. Should you try the keto diet? Harvard Medical School
8. Marcelo Campos, Ketogenic diet: Is the ultimate low-carb diet good for you?; Harvard Medical School
9. Refractory Epilepsy; Cedars Sinai
10. Ketogenic diet; NHS
11. Ketogenic Diet; Epilepsy Society
12. Daniela D.Weber et al.; Ketogenic diet in the treatment of cancer – Where do we stand?; Science Direct
13. Ketogenic diet; The Royal Children’s Hospital Melbourne
14. Michael S Duchowny; Food for Thought: The Ketogenic Diet and Adverse Effects in Children; NCBI
15. Ketogenic diet for epilepsy; Missouri Department of Health and Senior services
16. Ketogenic Diet for Seizures in Children; Stanford Children’s Health

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Pooja Parikh