16 Symptoms Of Lupus In Children, Types, Causes & Treatment
The proper medication dosage can help manage its symptoms and reduce further risks.

In This Article
Lupus in children is a systemic autoimmune disease where a child’s immune system attacks its tissues and organs, such as the skin, joints, heart, brain, and kidneys. Its precise cause is unknown, but environmental and genetic factors play a role. The condition affects ten in one million children every year. About 15 to 20% of lupus patients have a childhood onset of the disease (1).
Lupus is often difficult to diagnose as its symptoms are similar to several other illnesses. Further, pediatric onset may cause more severe illness and organ damage over time. The symptoms and flare-up of lupus can be managed with medications. Prevention isn’t possible, but you can manage the condition better by avoiding the factors that trigger the symptoms.
Read on to know more about the types, possible causes, symptoms, diagnosis, and treatment for lupus in children.
Types Of Lupus
Lupus can be of four types based on its clinical features and cause (2).
- The systemic lupus erythematosus (SLE) is the most common type of lupus that affects the whole body system and multiple organs of the body.
- The cutaneous lupus erythematosus (CLE) involves only the skin, and you may notice sores or rashes in the sun-exposed areas, such as the face, neck, scalp, arms, and legs. It is basically a butterfly type of rash on the face.
- Drug-induced lupus is caused by the intake of certain drugs and usually disappears once the person stops taking the triggering medication.
- Neonatal lupus is temporary lupus caused by autoantibodies from the mother reaching the baby through the placenta. It is seen in newborns and usually disappears within a few months without causing severe damages.
If your child had any past incidence of drug-induced lupus, let the doctor know before they prescribe medication. The doctor may prescribe drugs that do not cause drug-induced lupus.
Causes Of Lupus In Children
The exact cause may not be known in many cases. However, the following factors may increase the risk of developing lupus in children (3).
- Genetic factors
- Viral infections
- Medications, such as procainamide and hydralazine
- Physical or emotional stress
- Certain hormones, such as estrogen
Lupus could be a result of a combination of genetic and environmental factors. Girls tend to be at a higher risk due to the estrogen hormone. Nevertheless, some children may not develop the condition despite having the risk factors, while some may have lupus without any risk factors.
Signs And Symptoms Of Lupus In Children
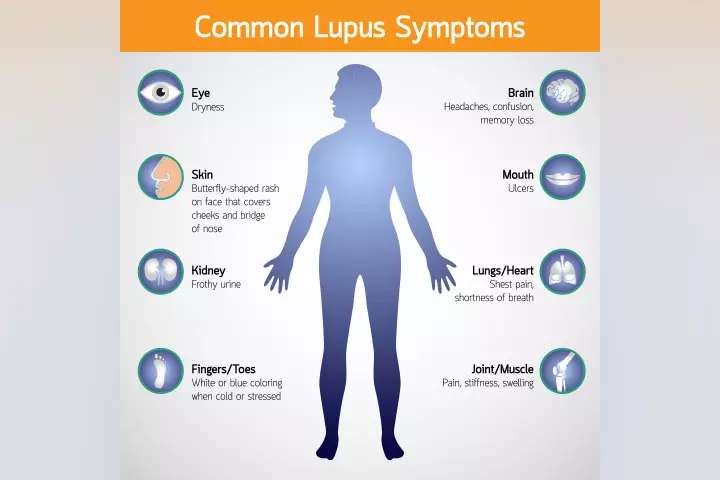
The signs and symptoms may vary in each child, depending on the severity and affected organ or tissue. These may include (4):
- Skin rashes on the body and face. Butterfly rash on face
- Fever
- Joint pain (Arthralgia)
- Photosensitivity. Rashes developing on exposure to sun
- Fatigue and tiredness. Muscle aches
- Muscle aches
- Oral, nasal, and throat sores
- Swollen lymph nodes
- Weight loss
- Hair loss or alopecia
- Tingling, pain, cold, and numbness on fingers or toes (Raynaud’s syndrome)
- Increased infections
- Anemia (low red blood cell count)
- Seizures and other neurological symptoms
- Kidney problems varying from low urine output, acute glomerulonephritis to renal failure
- Inflammations, such as pericarditis, pleuritis, and peritonitis
These symptoms and signs can also be seen in other diseases. Consult a pediatrician for the exact diagnosis and treatment of lupus.
Diagnosis Of Lupus In Children
Lupus diagnosis can be suspected based on the symptoms and physical examination. The following tests are often ordered to confirm the diagnosis (5).
- Antinuclear antibodies (ANA) in the blood
- Blood cell count
- Urinalysis
- Kidney and liver function test
- Skin and kidney biopsy
Doctors may order additional tests such as imaging tests, including MRI, CT, echocardiography, and chest X-ray, to determine organ involvement.
Your child may also be referred to a specialist, such as a dermatologist for cutaneous lupus or rheumatologist for joint problems, for evaluation or treatment based on the organs and tissues involved.
Treatment For Lupus In Children
There is no specific cure for lupus. However, symptoms can be managed with medications. The treatment options may vary based on the organs involved. The following medications are often prescribed to control common symptoms and reduce the severity of the disease (6).
- Corticosteroids, such as prednisone, to reduce inflammatory reactions
- NSAIDs (nonsteroidal anti-inflammatory drugs), such as ibuprofen and naproxen, for pain, fever, and swelling
- Acetaminophen for pain
- Antimalarial drugs, such as hydroxychloroquine, to reduce lupus flare-up as well as to reduce joint pains
- Immunosuppressants, such as azathioprine and methotrexate, to reduce autoimmune reactions
- Biologics, such as belimumab and rituximab, to minimize lupus symptoms
These drugs may cause some side effects, such as stomach upset and allergic reaction. Although some of them are available over-the-counter, taking them for a chronic condition without knowing the appropriate dosage could increase the risk of side effects.
Always seek medical consultation for long-term drug therapy for lupus. Doctors may add other medications in prescription to protect the stomach lining.
Prevention For Lupus In Children
Although all cases of lupus cannot be prevented, the following tips may prevent incidences of lupus in some children or rather reduce flareups (6).
- Reduce stress
- Get enough rest
- Take part in regular physical activity
- Stick to a healthy diet
- Reduce sun exposure
- Avoid lupus-causing drugs
- Get vaccinated and practice hygiene measures to reduce viral infections
The above-mentioned measures may also prevent flare-ups in children with existing lupus symptoms. Lupus may persist for life, so your child requires follow-up visits and medications during a flare-up. You may contact their doctor sooner if you notice the recurrence of symptoms to begin immediate treatment and reduce the severity of the illness. Lupus is not a life threatening disease and can be easily managed with proper treatment and guidance.
Frequently Asked Questions
1. At what age is lupus usually diagnosed?
Although the symptoms might be present in childhood, lupus is usually diagnosed among individuals between 15 and 45, and it is more common in women than men (7).
2. What is the life expectancy of a child with lupus?
Recent studies have shown that the survival rate of children with systemic lupus erythematosus (SLE) might be between five to ten years. However, cumulative organ damage might be reported in at least 50% of individuals (8).
Diagnosing lupus in children can be tricky since its symptoms are similar to some other illnesses. Though the exact cause is unknown, genetic factors, viral infections, mental and physical stress, and hormones such as estrogen may lead to lupus in children. The symptoms may include skin rashes, arthralgia, tiredness, muscle aches, swollen lymph nodes, and hair loss. Although there is no effective treatment for lupus, the symptoms can be managed with corticosteroids, NSAIDs, acetaminophen, antimalarial drugs, and immunosuppressants. However, discontinue the medication and contact your doctor if your child experiences an upset stomach or allergic reactions.
Key Pointers
- Several factors can cause lupus in children, including genetic factors, viral infections, and stress.
- Some symptoms of the condition include rashes on the face and body, muscle ache, and fever.
- Though there is no specific treatment for lupus, medications can help manage the symptoms.
- Getting enough rest, physical activity, and healthy food can help prevent lupus in children.
References
2. What is lupus?;The National Resource Center on Lupus
3. Pediatric Lupus;The Children’s Hospital of Philadelphia
4. Lupus; Boston Children’s Hospital
5. Lupus and children; The National Resource Center on Lupus
6. Systemic Lupus Erythematosus (Juvenile); American College of Rheumatology
7. Lupus facts and statistics; The National Resource Center on Lupus.
8. Angelo Ravelli et al., Outcome in juvenile onset systemic lupus erythematosus; Current Opinion in Rheumatology (2005).

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Mubina Agboatwalla