Lyme Disease In Children: Causes, Symptoms And Treatment
Lyme disease is the most common vector borne infection frequently appearing in children of all ages. The disease is often seasonal and spreads through tick bites; however, the ticks do not cause the disease.
What causes Lyme disease in children? What would it feel and look like and how to deal with it? MomJunction answers all these questions and more about Lyme disease.
In This Article
What Is Lyme Disease?
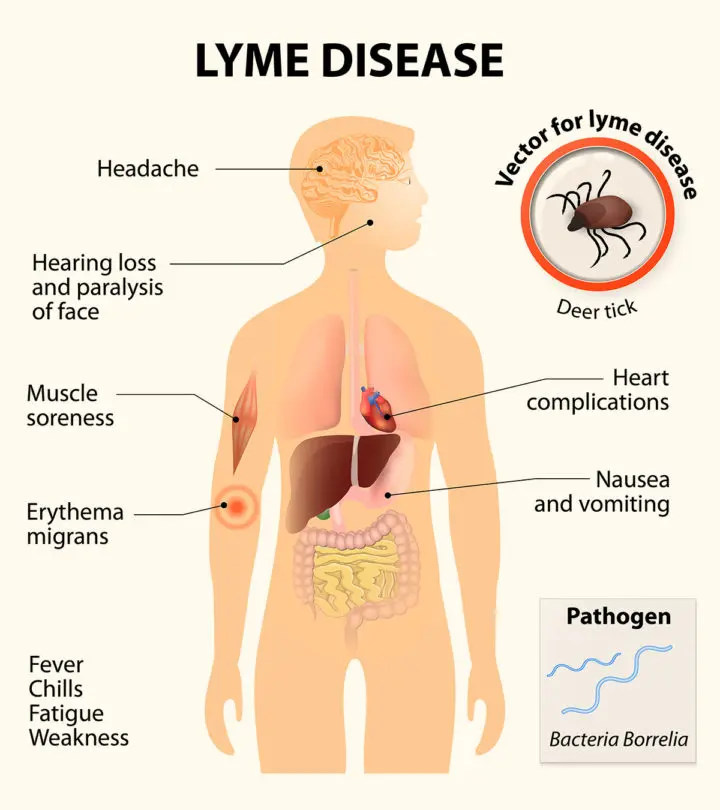
Lyme disease is a multisystem illness caused by bacteria Borrelia burgdorferi. The bite of the tick does not cause the infection but is just the carrier of it.
The bacterium uses tick of the genus Ixodes as a vector to transmit itself from animals to human beings. A child gets the disease when bitten by a vector tick with the Borrelia bacteria. The disease got its name from a town called Old Lyme in the US, where the condition was first reported in the year 1977.
How Common Is Lyme Disease?
According to various research studies, around 300,000 cases of Lyme disease are reported in the US every year (1). The disease is mostly found in the Northeast and upper Midwest with 14 states in this region accounting for 96% of the cases in the country. It is also commonly found in Europe and Asia. The disease has a seasonal character in a geographically endemic area, occuring in the period from May through November.
[ Read: Loss Of Appetite In Children ]
Factors That Increase The Risk Of Lyme Disease In Kids
Some risk factors can exacerbate the chances of a child contracting the disease:
- Active outdoor lifestyle: Ticks prefer living in wooded areas, low grasslands, and green fields. If a child spends time playing outdoors especially in green surroundings, then they are at a higher risk of being bitten by a tick.
- Having pets at home: Pets are prone to get ticks because of their thick fur. A tick can find its way into your home through your family pet.
- Type of tick: Not all types of ticks can transmit the bacteria. For instance, several ticks found in Australia do not carry the Borrelia bacteria. The most common ticks to transmit the Lyme disease are Black-legged deer tick and Western black-legged tick both of which are found in the US (2). The number of ticks laden with bacteria in a region can vary from 1 to 90%.
- The region of residence and season of the year: In the US, it is commonly seen in the Northeast and Mid-Atlantic states, Northern California, and the states of Wisconsin and Minnesota. The Lyme disease is the most common during spring and summer months.
The disease usually spreads through the bite of the immature tick called nymph although adult ticks can also transmit the bacteria.
According to the US Centers for Disease Control and Prevention (CDC), a child may get the Lyme disease when the tick attaches to their body for at least 24 hours. However, experts opine that bacteria can infect even with shorter duration. Hence look out for the symptoms if you see a tick on the child’s body.
What Are The Symptoms Of Lyme Disease In Children?
The symptoms may emerge 2-30 days (3) after the bite and appear in stages with increasing intensity.
First stage symptoms:
Early localized lyme disease refers to isolated erythema migrans and an undifferentiated febrile illness. A unique and earliest sign of Lyme disease is the appearance of the bull’s eye rash. It is a rash with a dark pink to red color center surrounded by a ring of the same color.
- The rash may appear a few days to weeks (average seven days) after being bitten by a tick. It has an average diameter of 13 to 15 cm.
- The bull’s eye rash may not itch and sometimes feels warm or may not cause any sensation at all.
- It can appear on any part of the body and not necessarily in the area where the tick bit.
- The rash is the first indicator that the child was bitten by a tick with the Lyme disease bacteria.
- The rash may persist for two to three weeks.
[ Read: Meningitis In Children ]
Second stage symptoms:
- The flu like symptoms (fever- usually low grade, chills and malaise) emerge over a few weeks to months after the tick bite. The most common symptom during this stage is an acute headache.
- Muscle and joints begin to ache. The child will also experience stiffness, like a stiff neck.
- There is a loss of appetite and a constant feeling of tiredness. The child becomes weak and lethargic.
- Swollen lymph nodes.
- Meningitis, which is an inflammation of the membranes covering the brain; other nervous system problems including Bell’s palsy, which is paralysis of the facial muscles.
- Acute inflammation of heart muscles and an increase in the heart rate.
- Inflammation of the eyes.
- Skin problems.
- Liver problems like development of hepatitis.
Third stage symptoms:
- The third stage symptoms of lyme disease are the most severe but only occur if all the earlier symptoms are not recognized timely. These symptoms usually emerge months or even years after being bitten by the tick.
- The child develops arthritis, which is a severe inflammation of the joints.
- A constant tingling sensation and pain in the limbs.
- The child may develop gross motor problems like coordinating different muscles of the body to perform an action.
- Problems with speech and memory.
- A research study noted that the prognosis of Lyme disease includes severe problems like behavioral changes and poor performance at school. In more severe cases, the child may develop seizures (4).
The second and third stage symptoms are the complications of Lyme disease that the child could have if you ignore the infection. The bull’s eye rash itself should alert you to take the child to a doctor.
How Is Lyme Disease Diagnosed?
The doctor uses the below steps to diagnose Lyme disease in children:
- Check the symptoms: The doctor checks for the tell-tale bull’s eye rash and the presence of any tick bites on the child’s body. Parents are asked about the child’s routine in the past few weeks to months to ascertain if the child could have been bitten by a tick.
- Blood test: The bull’s eye rash may not appear in 20-25% of Lyme disease cases, and in such cases, the doctor will have to rely on further analysis for accurate diagnosis. The blood test checks for the presence of Borrelia bacteria and antibodies against it. A blood check will make an accurate diagnosis of the disease.
The diagnostic tests for Lyme disease are complex and may require the services of a specialized laboratory.
[ Read: Skin Rashes In Children ]
How Is Lyme Disease Treated?
Antibiotic selection, route of administration as well as duration of the treatment are guided by the patient’s clinical manifestations and the stage of the disease. Common antibiotics prescribed for the treatment of Lyme disease against Borrelia burgoferi: are amoxicillin, doxycycline, and cefuroxime. Children with complications like cardiac and nervous problems are administered intravenous antibiotics along with other medications.
Prognosis Of Lyme Disease
Children treated with antibiotics will have a complete recovery. There are seldom any lasting consequences of the disease unless when the child develops further problems like those with the nervous and circulatory systems.
How To Prevent Lyme Disease In Children?
Stopping tick bites is the only way to prevent the illness because the bacteria do not spread from person to person. Here is how you can prevent tick bites:
- Dress the child in full-sleeved clothing when outdoors: When going into the woods or gardens, dress the child such that their hands and limbs are covered. A full-sleeved shirt and trousers may prevent ticks from latching on to the skin.
- Tie your child’s hair and put a cap: Ticks cannot fly or jump, but they can crawl on any surface. If your child has long hair, then tie it into a tight ponytail, and twist it to fit snugly through the strap of the cap. It prevents the hair from accidentally coming in contact with branches and rocks where a tick may reside.
- Walk through a clearing in the woods: Walk on forest trails with minimal surrounding thicket. It reduces your risk of encountering a tick.
- Use insect repellents: If you live in a tick-infested area, then use 10-30% DEET insect repellent spray to sprinkle it on the child’s clothing before they wear them. It is safer to apply insect repellents on the clothes than on the skin. Apply the insect repellents on clothes and leave them to dry for several minutes after application (6).
- Check your pets: Pets may bring ticks home. Therefore, check your pets for ticks and always give them a bath with an anti-tick, anti-parasite shampoo.
- Check for ticks on the body: Check your child for any ticks once you come back from tick-infested areas. Common hideouts of ticks are folds of the skin like underarms, folds of arms and legs, behind the ears, and places where the clothing elastic meets the body. Check the hair as well. If a tick bit the child but there is no tick on the body, then the bite will look like a small reddened area with a puncture mark at its center.
- Wash clothes in warm water: Soak the clothes in hot water for about 15 minutes before washing them after your return from outdoors. It can help remove and kill any tick that crawled onto the clothes.
Your child can also take a shower after returning from outdoors to remove any unattached ticks from the body. Of course, if you dressed the child appropriately, then you need not worry about it much. Nevertheless, if you find a tick, then you must promptly remove it.
[ Read: Hepatitis In Children ]
How To Remove A Tick?
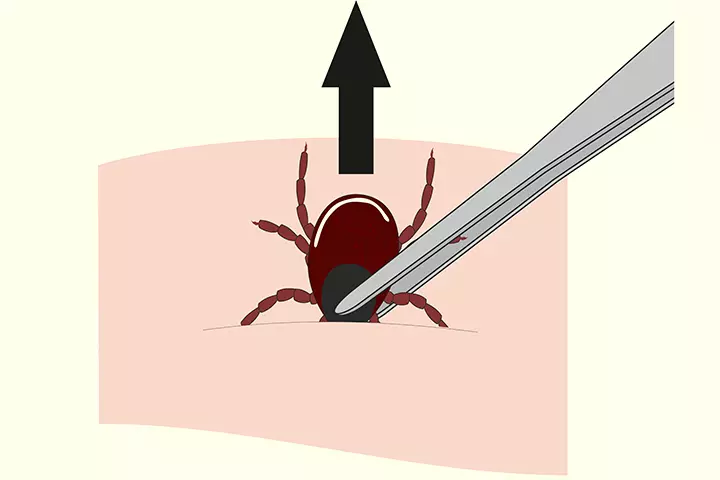
If you discover a tick on the child’s body, then follow these steps to remove it (7):
- Use fine-tip tweezers to grab the tick as close to the body as possible. If you grasp the tick by its belly, then you may rupture it.
- Once you have a good grip, gently pull the tick upwards with a steady pull. Do not jerk or twist the tick since it may cause it to break.
- The pressure will cause the tick to release its bite slowly. Be patient since it may take time.
- If you got the tick off the body, but it broke, then the mouthparts will still be attached to the body. Use the tweezer to remove the mouthparts gently. If you are unable to remove the tiny mouthparts, it is okay as they will fall off gradually.
- To kill any germs, dab the site with a cotton ball soaked in alcohol. You can also wash the bite with soap and water, and pat dry with a clean towel.
- Do not crush the removed tick. Store it in a sealed bag or container filled with alcohol, and take it to the doctor. Your doctor can check if the tick is of the type that can spread Lyme disease. Once your doctor is done with the assessment, make sure the tick is dead before flushing it down into the toilet.
Do not use home remedies like the application of nail paint, petroleum jelly or heat on the tick. They do not loosen the tick and may cause it to burrow firmly into the skin. A set of fine-tip tweezers is the best instrument to remove the tick.
Lyme disease may hold the potential to cause complications, but that happens only if you ignore the initial rash. Preventing the disease, both personal and environmental is easy since all you have to do is avoid the vector. Being watchful of ticks and prompt doctor consultation on getting bitten by a tick are the best ways to keep your child protected from Lyme disease.
Do you have an experience to share? Let us know in the comments section below.
References
2. About ticks and Lyme disease; Lymedisease.org.
3. Lyme borreliosis in Europe; WHO.
4. The stages and symptoms of Lyme sisease; Emerge Australia
5. Bloom et al., Neurocognitive abnormalities in children after classic manifestations of Lyme disease; The Pediatric Infectious Disease Journal
6. Preventing tick bites; Centers for Disease Control and Prevention
7. Tick removal; Centers for Disease Control and Prevention

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.