Medication When Breastfeeding: Is It Safe Or Unsafe?
Refer to LactMed or seek a prescription before taking any medications when breastfeeding.

Image: iStockphoto
In This Article
Several mothers use medications when breastfeeding and speculate if these drugs have any adverse effect on their baby’s health. Most commonly used medications, when used under guidance, cause no harm. Some drugs can get transferred to the baby via breast milk. However, these levels may not be high enough to have any harmful effects on babies.
Thus, the mother doesn’t have to cease breastfeeding in most cases. But then, if you are on certain medications, such as oral retinoids and anticancer drugs, you may have to stop breastfeeding. Therefore, nursing mothers must consult an expert before taking any medications.
Read on to learn more about the safe and unsafe medications for lactating mothers and ways to minimize their effects on the baby.
Do All Medications Pass Into Breast Milk?
Most of the medications present in a mother’s blood can pass into breast milk. However, the amount of medication may vary. Low levels of certain medicines in breast milk may not cause any risk in most babies. However, medications that can concentrate in the breast milk over time could be harmful though low doses are taken.
The following factors may affect the concentration of medications in breast milk (1).
- Maternal plasma concentration is directly related to the concentration of drugs in breast milk. This may be high in immediate hours after taking medications.
- Drugs’ ability to bind to maternal plasma protein may also affect breast milk levels. Unbound medications can quickly diffuse to breast milk.
- Small drug molecules may enter breast milk more quickly than high molecular weight drugs.
- Breast milk is slightly acidic than maternal plasma. So drugs that are weak bases, such as codeine, can easily reach the milk.
- Lipid-soluble drugs can easily be dissolved into the milk.
- Age of baby, time of feeding, and amount of breast milk fed may also influence the effects on the baby.
Each medication in each case must be considered separately due to these factors. The LactMed database of the U.S. National Library of Medicine may give general information about the safety of various drugs in breastfeeding mothers (2). You may also discuss the various factors that influence the transfer of the drug to breast milk with your doctor before beginning the medicine course.
What Medications Are Safe While Breastfeeding?
You may always seek a prescription to take any medications while breastfeeding. The following commonly used medications are found to be safe to use while nursing (3).
- Pain relievers such as ibuprofen (Advil, Motrin IB) and acetaminophen (Tylenol). Naprosyn (naproxen) and low-dose aspirin can be safe for short-term use.
- Antihistamines such as Allegra Allergy (fexofenadine) and Alavert or Claritin (loratadine).
- Medications reducing stomach acid production such as Tagamet HB (cimetidine) and Pepcid (famotidine).
- Antifungal medications such as Diflucan (fluconazole), Mycelex (clotrimazole), and Monistat 3 (miconazole).
- Antibiotics such as penicillin (amoxicillin, ampicillin), erythromycin, vancomycin, and cephalosporins (cephalexin or Keflex).
- Decongestants, such as Sudafed and Zyrtec D, can be used with caution since some compounds in these medications may decrease milk supply.
- Birth control pills such as mini-pills (progestin-only). Combined hormonal birth control pills containing estrogen can be used, but they may reduce milk production.
- Stool softeners for constipation such as Dicto or Collace (docusate sodium).
- Antidepressants such as Luvox (fluvoxamine), Paxil (paroxetine), and Zoloft (sertraline). You will want to monitor your baby for sleepiness, poor feeding or decreased weight gain.
- Antivirals such as acyclovir (Zovirax) and valacyclovir (Valtrex).
- Antacids such as Mylanta and Maalox.
- Local anesthetics such as Marcaine (bupivacaine) and lidocaine.
- Corticosteroids such as prednisolone and prednisone.
- Cardiac medications such as digoxin (Lanoxin) and verapamil (Calan, Verelan).
- Anticoagulants such as Coumadin (warfarin) and low molecular weight heparins.
- Bronchodilators for asthma such as terbutaline and albuterol.
- Insulin in low doses.
- Magnesium sulfate for seizures and other conditions.
- Antihypertensives such as methyldopa, nifedipine, and metoprolol (Lopressor).
- Topical creams for acne such as Avita, Renova, and Retin A (tretinoin).
- Thyroid replacement drugs such as levothyroxine and Synthroid.
Although these medications are known to be safe for lactating mothers, monitoring of the baby and dose adjustments are often required, depending on individual factors. Breastfeeding women can also get safely vaccinated with inactivated or live virus vaccines, except for the yellow fever vaccine and smallpox vaccine.
How To Take Medications While Breastfeeding?
The American Academy of Pediatrics recommends lactating mothers use a low dose and short course of medications when it is absolutely required since the effects of all medicines on breastfed infants are not fully clear. The following tips may help to reduce the risk of maternal medication effects on breastfed babies (1).
- Always inform the healthcare provider that you are breastfeeding before prescription and mention if your baby has any health issues. This may help the doctor prescribe alternative medications if the commonly used ones may impact nursing.
- Mothers with preterm babies should specify it since preemies may not be able to cope with certain medications as term babies due to less developed organ systems and low birth weight.
- Always use prescription medications and ask the doctor about the proper dosage and safety of over-the-counter medications if required.
- Take medications after breastfeeding the baby and breastfeed again after a gap of one or two hours. You may ask the doctor for suitable instructions since some drugs may require more time to clear from maternal blood.
- Once-a-day dose medications are often recommended if you have a few feeding sessions a day with a long gap between each of them.
- Use shorter-acting medications since they are eliminated quickly from the body.
- Look for any adverse effects in the baby, such as rashes, irritability, and sleepiness, for timely diagnosis of side effects.
- Expressing milk and storing it for a particular time is recommended before taking certain medications.
- Temporary suspension of breastfeeding is recommended while using cytotoxic drugs such as radiopharmaceuticals.
What Are The Medications To Avoid While Breastfeeding?
There are various drugs to avoid during nursing if alternative options are available. In some circumstances, medicines with fewer risks are prescribed, and the baby is closely monitored for effects.
The following drugs are contraindicated in lactating mothers (1).
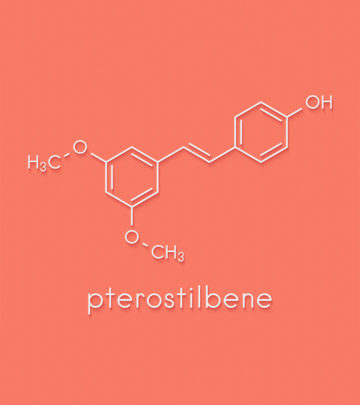
- Amiodarone may take a long time to metabolize, and the iodine molecule in it may affect the baby’s thyroid function.
- Retinoids may cause potential side effects in babies.
- Iodine in high doses may result in infant hypothyroidism.
- Gold salts may cause nephritis, rashes, and other hematological abnormalities.
- Antineoplastic may cause bone marrow suppression and leukopenia.
- Radiopharmaceuticals may cause adverse effects and are taken after a temporary suspension of breastfeeding.
- Lithium is given in unavoidable circumstances with constant monitoring of the baby for early detection of effects.
Although smoking may increase the risk of sudden infant death syndrome, nicotine replacement therapies are not an absolute contraindication to nursing. A high intake of caffeine during breastfeeding may also cause issues in babies. Caffeine may often be an additive in certain drugs.
Should You Stop Breastfeeding While Taking Medication?
Although exclusive breastfeeding is recommended for the first six months of life, some mothers are advised to discontinue breastfeeding if they require a long-term prescription of potentially harmful drugs. However, most medications are safe to take during nursing, and often the benefits may outweigh the risks.
Permanent or temporary cessation of breastfeeding is recommended in unavoidable circumstances. Expression of breast milk with breast pumps is often suggested for mothers taking certain medications. You may express and store the breast milk as per recommendations. It is essential to maintain the instructed timing of medicine and milk expression to avoid adverse effects on babies (3).
Permanent cessation of breastfeeding due to adverse effects of drugs is rarely required. Doctors may try to use an alternative method of treatment in most cases. In some conditions, if it is absolutely necessary, mothers are advised to stop breastfeeding and supplement with infant formula feed and begin weaning if the baby is older than six months.
The type and dosage of medicine prescribed during breastfeeding could vary due to several factors. Regular observation of the baby to determine adverse effects may be required in all cases. You may always consult your healthcare provider before taking medication while breastfeeding to know the best recommendations for your baby’s safety.
Frequently Asked Questions
1. Do I need to pump and dump after medication?
The types of medication you are taking can help you decide whether you need to pump and dump after medication. When on certain medications, your doctor may ask you to pump and dump your breastmilk for some time. It is done so that the drug does not pass from breast milk to your baby. For instance, several doctors ask mothers to pump and dump milk for 24 hours after receiving anesthesia (4).
2. How long should I wait to breastfeed after taking medicine?
Many medications prescribed during breastfeeding aren’t contraindicated. Thus, you don’t need to avoid breastfeeding your baby unless asked otherwise by your doctor. However, in some cases, the doctor may ask you to pump and dump or delay breastfeeding. For instance, if you are taking pain-relieving drugs, such as aspirin, you should try to breastfeed an hour or two after taking the dose. It will minimize the amount of the drug in your breast milk (5).
3. How long will drugs stay in breastmilk?
Almost all medications transfer into breastmilk. However, how much time a medicine stays in breastmilk varies from one medicine to another. For instance, analgesics, such as Sumatriptan have a short half-life of about two hours, which means you can avoid your baby’s exposure to this medicine if you pump and dump milk for up to eight hours after taking the medicine (6).
Always take the advice of a medical practitioner before consuming any medication while you are breastfeeding, as it can pass on to your baby. Pain relievers, antihistamines, and antibiotics are considered safe to be consumed while breastfeeding. However, the AAP suggests that you consume these medications in low amounts and short courses. It is advised not to stop breastfeeding your child while having medication until and unless it is advised by the doctor or under unavoidable circumstances.
Key Pointers
- Most medication present in maternal blood may pass into breast milk.
- Certain medications known to be safe when breastfeeding are pain relievers, antifungal medications, antibiotics, and birth control pills.
- Avoid medicines such as amiodarone, retinoids, gold salts, and iodine in high dosage.
- Ensure to consult a doctor before consuming any medication, consume only after a couple of hours of breastfeeding the baby, and keep a check on the dosage.
References
2. Drugs and Lactation Database (LactMed); U.S. National Library of Medicine
3. Breast-feeding and medications: What’s safe?; St. Clair Health
4. Benjamin Cobb et al; Breastfeeding after Anesthesia: A Review for Anesthesia Providers Regarding the Transfer of Medications into Breast Milk; NCBI
5. Breastfeeding and Drugs; Queensland Government
6. Drug Safety in Lactation; New Zealand Medicines And Medical Devices Safety Authority

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Julie Matheney