Tracheomalacia In Babies: Causes, Symptoms And Treatment
The symptoms of the condition may improve with age, and it is treated based on severity.
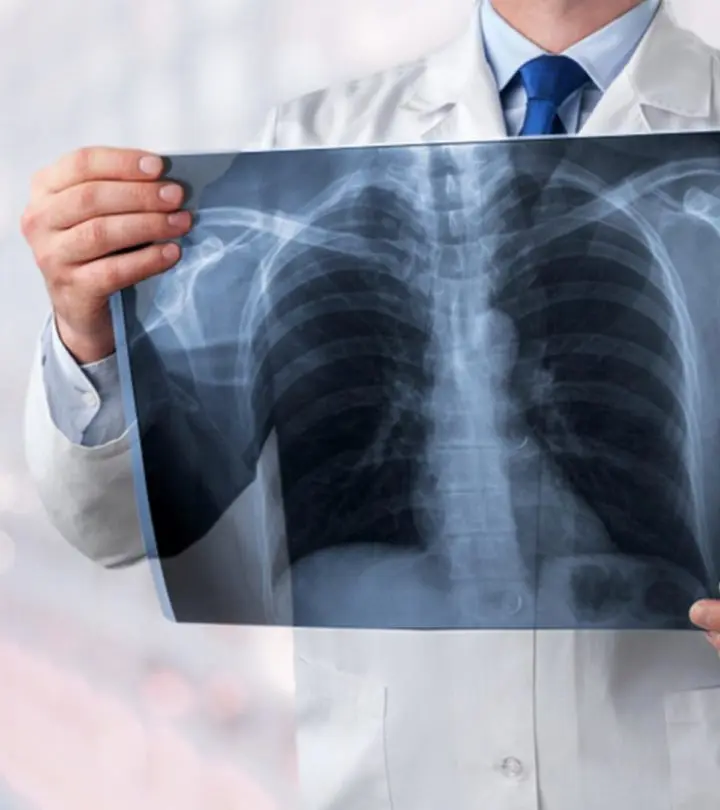
Image: Shutterstock
In This Article
Tracheomalacia in babies is a rare condition that could occur when the cartilage of the trachea (windpipe) has not developed properly. As a result, the trachea’s walls could become flaccid, and the soft cartilage cannot retain an open windpipe during exhalation, leading to trouble breathing. In some cases, pressure on trachea walls due to surrounding blood vessels may collapse the trachea (1) (2).
Read on to know more about the possible causes, signs, ways to diagnose and treat tracheomalacia in babies.
Types Of Pediatric Tracheomalacia
Tracheomalacia can be congenital (since birth) or acquired later. Pediatric tracheomalacia is classified into the following two types based on the time of occurrence (2).
- Type 1 Tracheomalacia (Primary tracheomalacia): Type 1 tracheomalacia is when the baby has congenital tracheomalacia. The baby is born with defects in the cartilage that supports the trachea.
- Type 2 Tracheomalacia (Secondary tracheomalacia): Type 2 tracheomalacia results from airway compression due to an airway injury. Trapped objects, repeated infections, or when the baby has a tracheostomy tube inserted for a very long time are some common risk factors.
Causes Of Tracheomalacia In Babies
The exact cause of primary tracheomalacia is not known since it is congenital (1). It may be affected by genetic factors.
The following conditions may cause secondary tracheomalacia in babies (1) (3) (4).
- Heart defects such as vascular rings
- Blood vessels abnormalities
- Skeletal abnormalities
- Large neck swellings
- Internal structures (tumors, cysts, and other growths) that push and narrow the trachea
- Recurrent infections
- Tracheostomy tubes
- Previous treatment for esophageal atresia (a birth defect where the baby’s food pipe is not well developed)
Symptoms Of Tracheomalacia In Babies
The following are the common symptoms of tracheomalacia (2) (3).
- Breathing difficulties that get worse with crying, feeding, or during episodes of cold
- Choking during feeding
- Cough
- High-pitch breathing
- Stridor (breathing noises) that may change with changes in positions
- Apnea (pause in breathing) and cyanosis (bluish discoloration of nails and skin around the mouth)
- Frequent airway infections such as pneumonia or bronchitis because of the baby’s inability to cough
- Recurrent noisy coughing
- Extended respiratory infections
- Difficulty in breathing during exertion or activities
Diagnosis Of Tracheomalacia
Tracheomalacia is often misdiagnosed as asthma, recurrent croup, or noisy breathing (3). The misdiagnosis is a result of the clinical overlap of symptoms and because diseases, such as asthma and croup, are more common than tracheomalacia.
Your baby’s healthcare provider may order one or more of the following tests to confirm tracheomalacia in your baby (2).
- Bronchoscopy: A small thin tube with a camera is inserted into the baby’s trachea through the mouth to aid the doctor in examining the trachea while the baby breathes.
- Laryngoscopy: It is a procedure similar to and performed in conjunction with bronchoscopy, but it evaluates the voice box and the upper airway.
- Airway fluoroscopy: It is a type of X-ray that shows the movement of the cartilage in the trachea.
- Esophogram: It is an X-ray that helps view vascular rings.
- Pulmonary function tests: This test shows the amount of air a baby can inhale and exhale.
- Endoscopy (Gastroscopy): A small thin tube with a camera is inserted into the baby’s mouth to examine the esophagus, stomach, and the beginning of the small intestine. The test is done to rule out gastrointestinal problems and defects.
- Computerized tomography (CT) scan and Magnetic resonance imaging (MRI): These are advanced scans, which are done if other tests are inconclusive or if the baby is suspected of having other problems, such as other congenital defects.
Treatment For Tracheomalacia In Babies
Tracheomalacia usually gets better as the baby grows older, and the symptoms may significantly reduce by 18 to 24 months. The treatment plan for tracheomalacia will depend on the severity of the condition.
The doctor may follow the following treatment protocol (2).
- Most babies respond well to humid air, monitored feedings, and appropriate antibiotics for infections.
- The doctors may prescribe medicines to help in airway clearance, such as ipratropium bromide.
- Nebulised saline drops are given to thin the secretions of the airways.
- Chest physiotherapy might be suggested to clear the mucus from the chest and minimize the chances of infections.
- Some babies may require respiratory support from devices, such as positive pressure ventilation (BiPAP or CPAP). The baby would have to wear a mask over the nose and mouth so that the air can be pushed gently into the lungs.
- In a few cases, a baby may need a tracheostomy. Tracheostomy is a process in which a tube is put into a hole in the baby’s neck to allow mechanical ventilation until the baby outgrows the problem.
- In severe cases, a baby may need surgery to stabilize the airways. The type of surgery will depend on the underlying cause of trachea collapse and the severity of the symptoms.
Possible Complications In Babies
Breathing problems and aspiration pneumonia due to inhalation of milk or food are common complications of persistent or untreated tracheomalacia. Infants with congenital tracheomalacia may already have other congenital defects, which may be exacerbated by tracheomalacia. Some of the common congenital defects and problems noted are:
- Congenital heart diseases
- Developmental delay
- Gastroesophageal reflux
- Esophageal abnormalities
When To Call The Doctor?
Primary tracheomalacia (congenital tracheomalacia) may be diagnosed soon or within a few hours after birth while you are still at the hospital. Secondary tracheomalacia, which may occur due to injuries or infections, may show symptoms that warrant prompt medical care (5) (6).
Consult a doctor if the baby shows the following signs and symptoms.
- Inability to swallow milk or formula
- Rapid breathing or labored breathing
- Frequent choking on milk or formula
- Refusal to feed or lack of interest in feeding
- Noisy breathing for several days
- Pauses in breathing that last more than ten seconds
- Skin turns blue
- Skin around the neck and chest retracts tightly with each breath
- Poor weight gain and lethargy
Frequently Asked Questions
1. Can tracheomalacia cause sleep apnea?
There has been a study that has reported the occurrence of sleep apnea related to tracheomalacia. However, it is advised to consult the doctor regarding the same for a proper diagnosis and treatment (7).
2. Is tracheomalacia the same as laryngomalacia?
No. Although tracheomalacia and laryngomalacia are conditions related to the windpipe, laryngomalacia refers to the condition affecting the tissues above the voice box. In contrast, tracheomalacia refers to the weak and affected tissues in the windpipe (8).
Tracheomalacia in babies is a rare condition. The disease severity may vary from mild, moderate, severe, or fatal cases (2). The condition is very commonly misdiagnosed. Therefore, a subject matter expert and the correct use of all diagnostic tools play an important role in its management. The condition usually gets better as the baby grows older. Severe conditions may need an aggressive treatment approach, and your healthcare provider will guide you regarding the long-term management and repercussions.
Key Pointers
- Tracheomalacia in babies may be either congenital or occur due to other issues such as heart defects, skeletal problems, large neck swellings, etc.
- Breathing problems, choking, coughing, etc., are some of the many symptoms of this condition in babies.
- Contact the doctor immediately if your child shows signs such as labored breathing, inability to swallow milk or formula, bluish discoloration of the skin.
References
2. Tracheomalacia; The Children’s Hospital of Philadelphia
3. Tracheomalacia; Boston Children’s Hospital
4. Santoshi Kurada et al., Management of tracheomalacia in an infant with Tetralogy of Fallot; Indian Journal of Anesthesia
5. Tracheomalacia; Cincinnati Children’s Hospital Medical Center
6. Tracheomalacia – congenital; U.S. National Library of Medicine
7. Hiren Mazumdar et al., Obstructive sleep apnea due to extrathoracic tracheomalacia; PubMed Central
8. Laryngomalacia; Cleveland Clinic

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Elna Gibson