How Ovarian and Antral Follicles Predict Fertility
Tests involving these follicles can help determine fertility and some ovarian disorders.

Image: Shutterstock
In This Article
The ovary’s basic units are ovarian and antral follicles. An ovarian follicle contains an oocyte (egg) that can mature and ovulate into an embryo, but an antral follicle, also called a Graafian follicle or a tertiary follicle, is an ovarian follicle in a later stage of folliculogenesis (maturation of the ovarian follicle).

Your chances of conceiving are determined by the number of ovarian follicles you have, either naturally or through assisted reproductive therapies such as IVI and IVF.
Read on to know about ovarian follicles and their relationship to fertility.
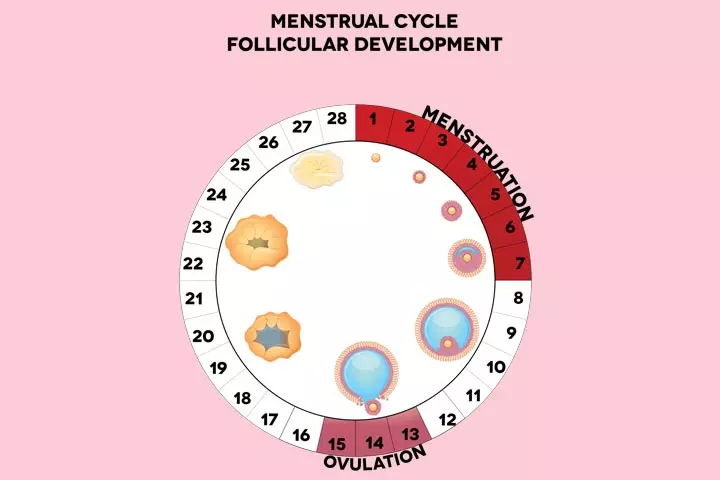
Role Of Follicles In The Menstrual Cycle
The menstrual cycle has two primary phases, the follicular phase and the luteal phase.
During the follicular phase, the antral follicles in the tertiary stage begin a process that leads to ovulation. While several follicles are stimulated, only one follicle matures into an egg (1). If you are on fertility drugs, several follicles may reach ovulation.
Follicles are responsible for (2):
- nourishing and protecting the oocyte or egg.
- releasing reproductive hormones, estrogen, and inhibin that signal pituitary and hypothalamus to regulate follicle-stimulating hormone (FSH), gonadotropin-releasing hormone (GnRH), and Luteinizing Hormone (LH).
- transforming into a corpus luteum, which secretes progesterone and estrogen.
Follicle Development Explained
Hormonal signals trigger the follicle development, which then mature and form a fluid-filled cavity, called the antrum, adjacent to the oocyte. These follicles with antrum are now called antral follicles, and they could be visible in an ultrasound. However, one cannot know the exact number of follicles present in a ovary and tests can only indicate the state of ovarian reserves, that is the number of eggs left by evaluating the size of ovary, number of antral follicles and anti-mullerian hormone.
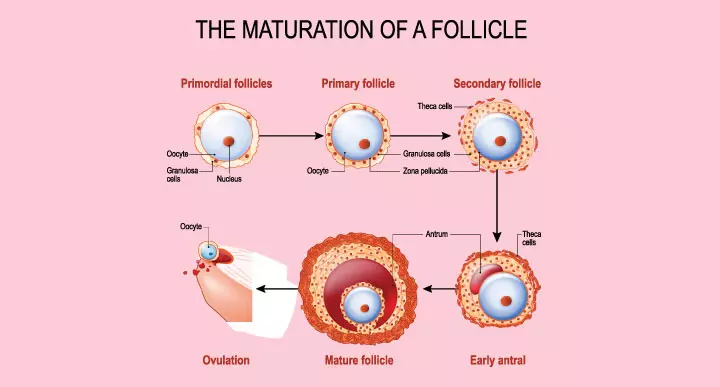
Folliculogenesis: The Stages of Follicular Development
The follicular development begins when the ovaries are first formed in the fetus. Around this time, there are only primordial follicles in the ovaries. They remain in a sleeping stage for several years until they enter into a growth pattern at puberty. It takes anytime between six months and one year for a primordial follicle to turn into a pre-ovulatory follicle. At every stage of development, most of the follicles enter into a growth pattern that ends in either death (apoptosis) or ovulation (where the egg leaves the follicle) (3) (4).
Stages of development
- Primordial follicles: In this stage, all the ovarian follicles are within the ovaries of a newborn girl
- Primary follicles: In this stage, a few primordial follicles turn into primary follicles every day, beginning from puberty until menopause.
- Secondary follicles: In this stage, the addition of theca cells, the endocrine cells that are responsible for secreting hormones, takes place.
- Tertiary follicles (antral follicles): In this stage, the antral follicles, which contain a fluid-filled cavity (antrum), become visible through transvaginal ultrasound.
- Graafian follicle: This is a relatively large follicle also called as dominant follicle that ovulates. Generally, only a couple of tertiary follicles mature.
- Corpus luteum: This is not a follicle anymore. It develops from a broken follicle that had released an egg and sustains early pregnancy (5).
What Are Antral Follicles And How Do They Predict Fertility?
Primordial follicles start to mature and grow larger. One of the later stages is the tertiary stage, during which a follicle accumulates fluid in the intracellular spaces, and merges to form an antrum. Follicles containing antrum are known as antral follicles (6).
The number of antral follicles present in the ovaries could give the potential number of eggs remaining. Antral follicles usually produce a hormone called anti-mullerian hormone (AMH) that circulates in the blood. Ovarian reserves are evaluated by measuring the level of AMH in the blood (7).
What Is An Antral Follicle Count Test?
Antral follicle count (AFC) or basal antral follicle count is a fertility test performed to check a woman’s ovarian reserve or remaining egg supply. The antral follicle is viewed, measured, and counted on days 2, 3, and 5 of the menstrual cycle using transvaginal ultrasound. The follicles measuring 2 to 10 mm in diameter are generally considered (8).
The healthcare practitioner may also suggest this test for other reasons:
- To diagnose primary ovarian insufficiency (premature ovarian failure) that could happen due to genetic disorders, autoimmune diseases, metabolic disorders, or toxins, such as smoke and chemicals (9).
- To diagnose polycystic ovary syndrome (10)
- To determine your fertility level in relation to your age
How Many Antral Follicles Are Normal In Each Ovary?
According to a study conducted on normal women with proven fertility, antral follicle counts were closely associated with their chronological age. The women who were included in this study had met all of the below criteria (6):
- Regular menstruation with cycle length varying between 21 and 35 days
- At least one pregnancy carried till full-term
- Conception within one year of unprotected intercourse
- No history of ovarian surgeries or ovarian abnormalities
- No history of endocrinological diseases
- Stopped hormonal contraception before two months of the study
The antral follicle count is obtained by counting the follicles in each ovary and summing them up. The AFC in the different age ranges are as follows (6):
| Age | Lowest AFC | Average AFC | Highest AFC |
|---|---|---|---|
| 25–34 years | 3 | 15 | 30 |
| 35–40 yea | 1 | 9 | 25 |
| 41–46 years | 1 | 4 | 17 |
Antral follicle count naturally comes down as you age. An abnormally high count may indicate polycystic ovarian syndrome (PCOS), while a low count may indicate premature ovarian failure (11).
Size Of Follicle At Ovulation
A mature follicle at the time of ovulation usually measures around 18 to 36mm (12). The doctor usually monitors the follicle size and its development through transvaginal ultrasound at the time of fertility treatments.
What Does Having A Lot Of Follicles Mean?
You are likely to release more eggs if you have a lot of follicles. Likewise, the chance of releasing healthy eggs increases, and it might result in a successful conception.
What Happens To Follicles After Ovulation?
Follicles transform into corpus luteum after ovulation. It is formed from a broken follicle without an egg, secretes progesterone and is responsible for regulating the menstrual cycle and pregnancy (5).
Frequently Asked Questions
1. How many follicles should I have during an IVF cycle?
Around 15 follicles is an acceptable number for IVF treatments. During IVF, your fertility specialist will continuously monitor the ovarian follicles. Once they reach 18 to 20 millimeter in diameter, they are aspirated using an ultrasound-guided needle. This releases the mature eggs, which are then collected and fertilized via in vitro fertilization (IVF) (13).
2. Can follicles in an ovary cause pain?
In some cases, a follicle does not release an egg for ovulation and might turn into a follicular cyst. Although relatively harmless, it can cause swelling and pelvic pain (14).
3. How many follicles should I have for a Clomid cycle?
You may need one or two mature follicles for a Clomid cycle. Every mature follicle could release an egg that is likely to fertilize.
4. How many follicles do I need for Gonadotropins or IUI cycle?
You may need one or two mature follicles for gonadotropins or IUI, because a higher number of follicles could mean multiple pregnancies
5. Can I get pregnant with small follicles?
Smaller follicles are less likely to yield a mature egg, and even if they do, embryos derived from them have a lower potential for implantation (15).
6. Does the antral follicle count include both ovaries?
Average antral follicle count (AFC) includes the number of follicles in both right and left ovaries. However, it is possible to say how many antral follicles are present in each ovary. It is also possible to count antral follicles based on the size on ultrasound examination (16).
Do not worry about the count and size of ovarian follicles. Knowing that you have a low AFC can cause you unnecessary worry. Talking to your doctor may ease your worries and following their medical advice will help you through the journey.
Key Pointers
- An ovarian follicle contains an egg that can mature and ovulate.
- When the ovarian follicle reaches the maturation stage (later stage of folliculogenesis), it is called antral follicles.
- The number of antral follicles in the ovaries indicates the potential number of eggs remaining (woman’s ovarian reserve).
- Fertility of a woman can be estimated by measuring the remaining egg supply through a fertility test called antral follicle count.
- An unusually high antral follicle count indicates polycystic ovarian syndrome, while a low count indicates premature ovarian failure.
References
2. Julie E. Holesh and Megan Lord.; Physiology, Ovulation; Treasure Island (FL): StatPearls Publishing (2020).
3. Gregory F. Erickson; Follicle Growth and Development; The Global Library of Women’s Medicine (2008).
4. F. Guerin; Folliculogenesis And Ovulation; Geneva Foundation for Medical Education and Research (2019).
5. R. Baerwald, et al.; Form and function of the corpus luteum during the human menstrual cycle; Ultrasound Obstet Gynecol (2005).
6. J. Scheffer ,et al.; The number of antral follicles in normal women with proven fertility is the best reflection of reproductive age; Human Reproduction (2003).
7. Kannamannadiar Jayaprakasan, et al.; A prospective, comparative analysis of anti-Müllerian hormone, inhibin-B, and three-dimensional ultrasound determinants of ovarian reserve in the prediction of poor response to controlled ovarian stimulation; PlumX Metrics (2010).
8. Shivi Jain; Antral Follicle Count as Predictor of Ovarian Reserve; ARC Journal of Radiology and Medical Imaging (2017).
9. Primary Ovarian Insufficiency; U.S. Department of Health and Human Services National Institutes of Health
10. Polycystic ovary syndrome; NHS (2019)
11. Paolo Beck-Peccoz and Luca Persani; Premature ovarian failure; Orphanet Journal of Rare Diseases (2006).
12. Eze CU, et al.; Prediction of Normal Ovulation by Sonographic Folliculometry Involving Natural Cycles among Women in Ojo, Southwest Nigeria; West Indian Med J. (2015).
13. Martin M. Quigley, et al.; Follicular size and number in human in vitro fertilization; The American Fertility Society (1982).
14. Causes -Ovarian cyst; NHS (2019)
15. Revelli A, et al.; A critical review of bi-dimensional and three-dimensional ultrasound techniques to monitor follicle growth: do they help improving IVF outcome; Reprod Biol Endocrinol (2014).
16. The number of antral follicles in normal women with proven fertility is the best reflection of reproductive age; Oxford Academic

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Priya Shukla