Postpartum Cardiomyopathy (PPCM): Symptoms And Treatment
Avoiding cholestrol-rich foods and regular exercise can prevent this condition.
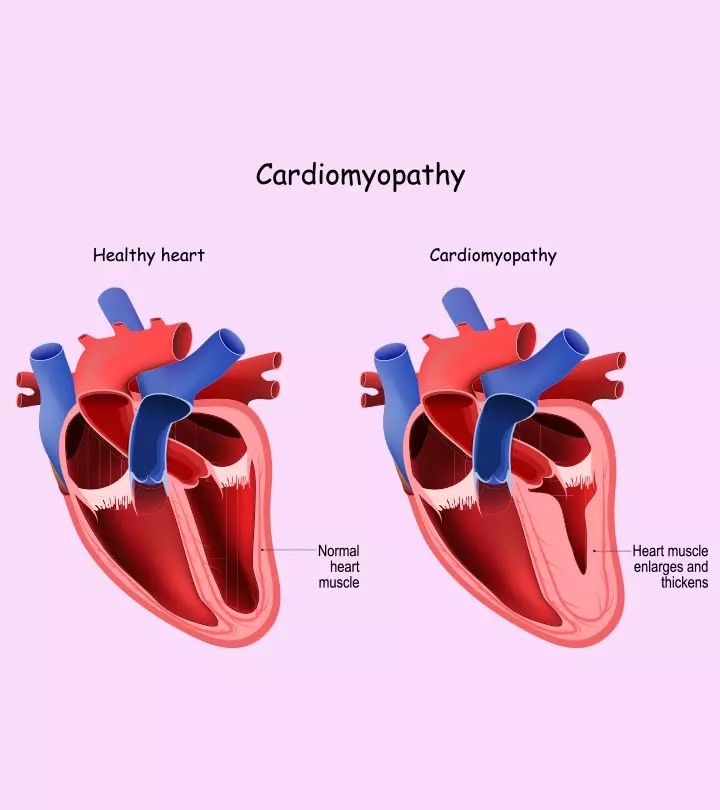
Image: iStock
In This Article
Postpartum cardiomyopathy or peripartum cardiomyopathy (PPCM) is a rare but severe heart condition where the heart grows larger and weaker due to congestion. These changes in the heart’s anatomy reduce its capacity to pump blood, ultimately reducing the oxygen supply to the organs.
It can cause serious health complications to affect you and your unborn baby’s overall health. Generally, PPCM affects pregnant women from the last month of pregnancy to five months postpartum. Hence, it is crucial to watch for the warning signs of the disease in the latter half of pregnancy.
Read on to learn more about postpartum cardiomyopathy and its causes, symptoms, treatment, and long-term considerations.
Causes And Risk Factors Of Postpartum Cardiomyopathy
The cause of postpartum cardiomyopathy is not known. A study shows the occurrence of postpartum cardiomyopathy in 10.3 patients per 10,000 live deliveries (1).
Some of the likely causes of postpartum cardiomyopathy are (2):
- Viral myocarditis (inflammation of heart muscle)
- Nutritional deficiencies
- Autoimmunity
- Microchimerism (small cells transferred from one genetically distinct individual to another)
- Hemodynamic stress
- Vascular dysfunction (abnormal condition of blood vessels)
- Myocardial ischemia (blood flow is reduced to the coronary artery of the heart)
- Genetics and heredity
Some of the risk factors of peripartum cardiomyopathy are (2) (3):
- Multiple pregnancies
- Prolonged tocolytic use (used for treating preterm deliveries)
- Pregnancy at higher maternal age above 40 years
- Certain geographical regions, including Africa, Asia, Nigeria, and the southern US, have a higher disease prevalence.
Symptoms Of Postpartum Cardiomyopathy
Most symptoms are similar to dilated cardiomyopathy (DCM), such as ventricle dilation and systolic dysfunction. They are also similar to the symptoms of heart failure and are as follows (4) (5):
- Fatigue
- Palpitations in heart
- Increased urination at the night
- Shortness of breath
- Swollen ankles
- Swollen neck veins
Postpartum Cardiomyopathy Diagnosis
The symptoms of postpartum cardiomyopathy are similar to the symptoms experienced by pregnant women towards the end of the pregnancy (5). It can therefore make the symptomatic diagnosis of the disease difficult.
The diagnosis of postpartum cardiomyopathy is carried out as follows (4):
- Severe cases of postpartum cardiomyopathy may show symptoms of shortness of breath and swollen feet after delivery.
- A complete blood assay is performed to determine the functioning of vital organs and markers of heart injury.
- An examination with a stethoscope can assess the presence of fluid in the lungs, lung crackles, rapid heart rate, and abnormal heart sound.
- Further screening by echocardiogram can determine the functioning of the heart.
- A diminishing function of the heart is a sign of peripartum cardiomyopathy.
Criteria for conducting a diagnosis of peripartum cardiomyopathy are:
- Heart failure in the third trimester or postpartum
- Reduced heart pumping
- Unknown cause of heart failure with reduced ejection fraction (EF), determined through an echocardiogram
Treatment For Postpartum Cardiomyopathy
The management of PPCM is done by lifestyle modifications and medications (3) (6):
- Limit salt and fluid intake
- Diuretics are used to reduce fluid retention
- Restrict physical activity to reduce stress.
- Drugs, such as beta-blockers and ACEIs, are used to slow down the heartbeat and allow recovery time for the heart. However, these medications are contraindicated during pregnancy. Alternatives such as hydralazine and nitrates are generally used for disease management.
- Bromocriptine is a dopamine antagonist drug used to control prolactin secretion towards the end of pregnancy or postpartum. It is associated with favorable outcomes.
Long-Term Considerations For Postpartum Cardiomyopathy
Following the below lifestyle measures can avoid the recurrence of cardiac disease (6) (7).
- Joint MDT team to discuss risk of relapse
- Parents should avoid planning for another child (high risk of mortality dependent on cardiac ejection fraction.)
- Periodic monitoring of the heart with an echocardiogram and stress test can help determine the systolic function and left ventricle activity.
- Salt and fluid intake should be limited. The building up of fluid can be checked by measuring weight gain.
- Abstain from smoking and alcohol.
Complications Associated With Postpartum Cardiomyopathy
Some of the complications associated with postpartum cardiomyopathy are (3):
- Blood loss during cesarean childbirth might pose a risk to the PPCM patients. Vaginal childbirth is preferable.
- The risk of reoccurrence is around 56%, with a 12% mortality rate.
- Drugs, such as thiazides or frusemide used for pulmonazry congestion might cause placental hypoperfusion (reduced blood flow).
Prevention Of Peripartum Cardiomyopathy
Here are some measures that help you prevent peripartum cardiomyopathy (8).
- Avoid smoking and alcohol
- Maintain healthy weight by regular exercise and a nutritious diet
- Abstain from a high salt diet
- Avoid high cholesterol foods and keep a check on the blood cholesterol levels
- Maintain a stress-free lifestyle and maintain healthy blood pressure
Outlook for Postpartum Cardiomyopathy
Postpartum cardiomyopathy is a serious health condition. It might take from a week to several months to gain optimum recovery. However, following a healthy regime can help in a faster recovery.
Despite the complete recovery, it may be risky to plan for the next normal pregnancy. It may be feasible to have a viable pregnancy under the medication and doctor’s guidance.
Frequently Asked Questions
1. How common is cardiomyopathy in pregnancy?
Peripartum cardiomyopathy is rare in the United States, Canada, and Europe. The condition may be seen in around 1,000 to 1,300 women in the U.S. each year (4).
2. Is peripartum cardiomyopathy fatal?
Cardiomyopathy during pregnancy is uncommon but may have life-threatening consequences. However, about 50% of the women with the condition will have full myocardial recovery within six months of diagnosis, while others may have complications (9).
Peripartum cardiomyopathy is a severe congestive heart failure experienced in late pregnancy or after childbirth up to five months. It is difficult to diagnose as the symptoms are similar to the third-trimester pregnancy symptoms. Good management and advice from a doctor can help get a full recovery. However, it would help if you avoid subsequent pregnancies to reduce the reoccurrence.
Key Pointers
- Low blood pressure, fatigue, and weak heart palpitations could be signs of peripartum cardiomyopathy (PPCM).
- Medical professionals may suggest an electrocardiogram (ECG), complete blood assay, or assessment with a stethoscope to diagnose this condition.
- Some lifestyle modifications such as taking diuretics, beta-blockers, and reducing salt and fluid intake could help manage PPCM.
- Avoiding consumption of alcohol, reducing stress, and maintaining a healthy weight could help prevent PPCM.
References
- Postpartum Cardiomyopathy.
https://www.ncbi.nlm.nih.gov/books/NBK534770/ - Aetiology and risk factors of peripartum cardiomyopathy: a systematic review.
https://pubmed.ncbi.nlm.nih.gov/18722678/ - CSI position statement on management of heart failure in India.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6097178/ - Peripartum Cardiomyopathy (PPCM).
https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/peripartum-cardiomyopathy-ppcm - Emergency management of decompensated peripartum cardiomyopathy.
https://pubmed.ncbi.nlm.nih.gov/19561973/ - Peripartum Cardiomyopathy.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripartum-cardiomyopathy - Peripartum Cardiomyopathy.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.113.001851 - Prevention.
https://herheart.org/heart-conditions/prevention/ - Jennifer Lewey and Jennifer Haythe et al.; (2014); Cardiomyopathy in pregnancy;
https://pubmed.ncbi.nlm.nih.gov/25037522/#

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.