Postpartum Endometritis: Causes, Risks, Symptoms, & Treatment
Abdominal pain or abnormal vaginal discharge may indicate uterine infection and inflammation.
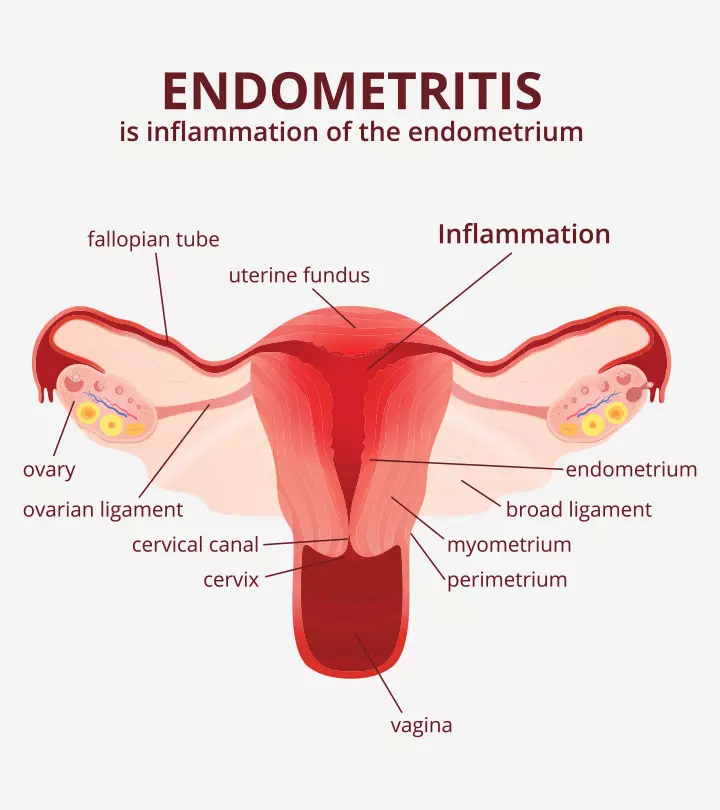
Image: Shutterstock
In This Article
Postpartum endometritis is a bacterial infection some women develop after childbirth. The infection usually affects the inner lining of the uterus (endometrium) (1). Though postpartum endometriosis isn’t a serious health condition, it often requires antibiotic therapy to avert complications. Early diagnosis and prompt treatment help in the early resolution of the problem.
Keep reading to learn more about postpartum endometritis and its causes, symptoms, risk factors, diagnosis, and treatment.
Causes Of Postpartum Endometritis
Both aerobic and anaerobic bacteria can cause endometritis. Some pathogens responsible for it are Clostridium, Staphylococcus, and Escherichia coli. Multiple bacteria can cause some endometritis. Most of these bacteria enter the endometrial cavity through the genital tract around delivery time.
Endometritis could also result after a miscarriage, abortion, or intrauterine device (IUD) insertion, or after any uterine instrumentation (e.g., hysteroscopy, dilation, and curettage) (2).
Signs And Symptoms Of Postpartum Endometritis
The most common symptoms of postpartum endometritis include fever and discomfort or tenderness in the vaginal area. The other signs and symptoms of endometritis may include (1) (3).
- Lower abdominal pain or swelling
- Foul-smelling vaginal discharge and bleeding
- Pain while urinating
If you notice any of these symptoms post-delivery (these can occur days to weeks following delivery), consult your doctor for evaluation and management to prevent future complications.
Risk Factors For Postpartum Endometritis
The common risk factors for postpartum endometritis include (1) (3) (4).
- Prolonged labor
- Improper prenatal care
- Prolonged gap between the rupture of the amniotic sac and delivery of the baby
- Internal examinations during pregnancy
- Manual removal of the placenta
- Using an intrauterine device
- Presence of meconium (fetal stool) in the uterus
- Bacterial infestation in the vaginal flora before delivery or labor
- Surgical site infections during delivery
Diagnosis Of Postpartum Endometritis
Postpartum endometritis is primarily diagnosed by observing the symptoms and conducting a thorough physical examination of the pelvis. The doctor may suggest urine or blood tests or vaginal swabs for microbiology for further confirmation (1) (4).
Treatment For Postpartum Endometritis
Most postpartum endometritis can be treated with oral antibiotics, although in severe cases, hospitalization for intravenous antibiotics may be required. Clinical findings suggest that the combination of clindamycin and gentamicin show positive results (5). Your doctor may also recommend ampicillin with other antibiotics. The choice of antibiotics typically depends on the results of your vaginal swabs, which will reflect the type of bacteria growing and the most appropriate antibiotics to treat it.
Note that you should only take these medications as per prescription, and it is essential to complete the whole course of antibiotics. Self-treatment may lead to serious repercussions.
Complications Of Postpartum Endometritis
According to the World Health Organization (WHO), women who have been exposed to bacteria causing chronic endometritis are prone to long-term problems, such as chronic pelvic pain, blocked or swollen fallopian tubes, secondary infertility, and risk of ectopic pregnancies. (6).
Postpartum endometritis can be treated with antibiotics if diagnosed at an early stage. However, if the infection is not diagnosed and persists, it may spread throughout the blood, leading to septicemia or even septic shock (1).
Prevention Of Postpartum Endometritis
Studies have shown that prophylactic antibiotic therapy could reduce the chances of postpartum endometritis by around 60% (7). However, this is not conducted usually and may be done only if your doctor prescribes it. In addition, proper prenatal care before delivery helps reduce the risk of postpartum endometritis (3).
Frequently Asked Questions
1. How common is postpartum endometritis?
Postpartum endometritis may be associated with around 1% to 3% of vaginal births and up to 27% of C-section deliveries (8).
2. Which antibiotics are used to treat postpartum endometritis?
Combining clindamycin and gentamicin antibiotics is recommended for treating postpartum endometritis (6).
Postpartum endometritis is a common infection occurring in women, especially those who had a cesarean mode of delivery. If diagnosed early, it can be cured with antibiotic treatment. However, if a timely diagnosis is not made, it may lead to serious health complications. Hence, consult your gynecologist if you suspect that you may be having postpartum endometritis.
Key Pointers
- Postpartum endometritis occurs if the bacteria enter the genital tract during delivery.
- Foul-smelling vaginal discharge, abdominal pain, fever, and pain while urinating are signs of postpartum endometritis.
- Postpartum endometritis is treated with antibiotics, and if left untreated, it can lead to complications such as chronic pelvic pain, blockage in fallopian tubes, and secondary infertility.
References
- Endometritis.
https://medlineplus.gov/ency/article/001484.htm - Endometritis.
https://www.ncbi.nlm.nih.gov/books/NBK553124/ - Postpartum Endometritis.
https://www.winchesterhospital.org/health-library/article?id=928910 - Puerperal endometritis
https://www.msdmanuals.com/en-in/professional/gynecology-and-obstetrics/postpartum-care-and-associated-disorders/puerperal-endometritis - Antibiotic regimens for postpartum endometritis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7050613/ - WHO recommendations for prevention and treatment of maternal peripartum infections.
http://apps.who.int/iris/bitstream/handle/10665/186171/9789241549363_eng.pdf;jsessionid=E31EC4D6582F57688D7A4E41B6CA1A25?sequence=1 - Prevention and treatment of postpartum endometritis.
https://pubmed.ncbi.nlm.nih.gov/12844449/ - Antibiotic regimens for postpartum endometritis.
https://pubmed.ncbi.nlm.nih.gov/12844449/

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.