Persistent Pulmonary Hypertension of the Newborn & Treatment
PPHN leads to a heart murmur or fast breathing and needs treatment to enhance oxygen supply.
In This Article
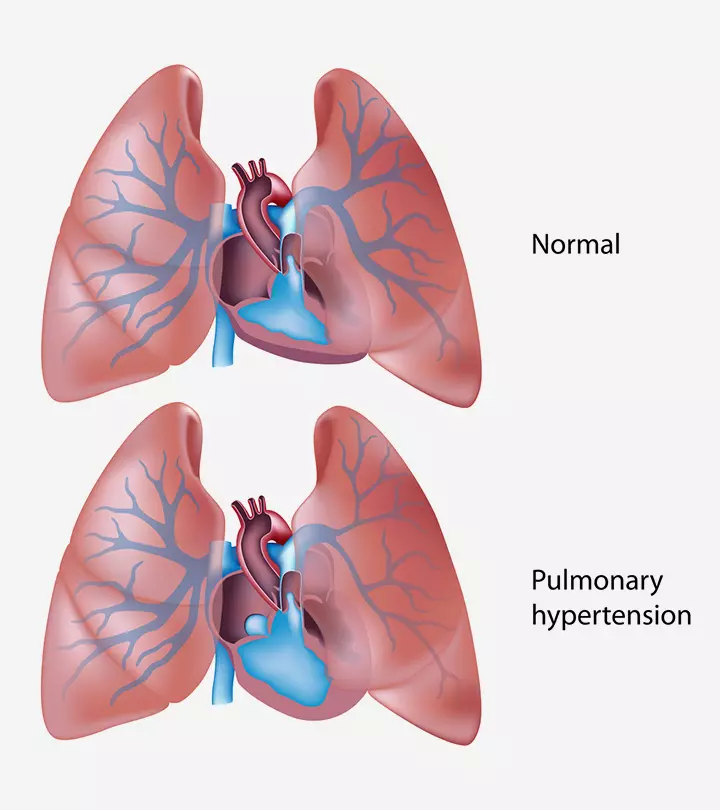
Persistent pulmonary hypertension of the newborn (PPHN) occurs when the blood in the infant’s lungs continues to circulate in the same way it did in the mother’s womb. The blood circulation of newborns with PPHN does not adjust to breathing outside the womb (1). As a result, a high amount of blood bypasses the lungs of the baby.
PPHN causes excessive blood pressure in the lungs of the newborn and even when the newborn is given 100% supplemental oxygen support, it may lead to reduced oxygen levels in the circulating blood. Since all body organs require a steady supply of oxygen-rich blood, failure to thrive enough oxygen may cause organs’ destruction.
Read on to know more about the causes, risk factors, symptoms, and complications of PPHN in newborns and how it can be treated.
How Does PPHN Occur?
The following points explain the pathophysiology of PPHN.
- While in the mother’s womb, the baby’s lungs do not exchange oxygen and carbon dioxide. The fetus receives oxygen through the umbilical cord, and the lungs need less blood supply.
- After birth, ideally, the circulation changes when the baby begins to inhale and exhale.
- This change in lung pressure helps in closing the fetal connections between the heart and the blood vessels. It helps in redirecting the blood to the lungs, and this blood flow to the lungs helps in the gaseous exchange.
- These changes may not occur in newborns who experience low oxygen levels or troubled breathing at birth. The fetus’ circulation sends most blood away from the baby’s lungs through the connections between the heart and large blood vessels.
- The blood vessels in the lungs remain constricted, reducing the flow of blood from the lungs. It ultimately leads to high blood pressure in the baby’s lungs and PPHN.
Several factors and conditions before and during a baby’s birth may a play role in causing PPHN. The following are the most probable causes (2).
- Problems with blood vessels in the lungs
- Abnormality of heart and lungs, such as diaphragmatic hernia, blocked heart valves, or smaller than usual lungs
- Difficulty in adjusting to the outside atmosphere after birth
- Meconium aspiration syndrome
- Lung or chest infections, such as pneumonia
- Bloodstream infections
Risk Factors Of PPHN
The following factors may increase a baby’s risk of developing PPHN (1).
- Difficult birth or birth asphyxia
- Postmature birth (full-term birth after due date)
- Maternal treatment with certain medications, such as non-steroidal anti-inflammatory medicines
- Maternal infections, such as streptococcal infection
- Babies with pneumonia or heart and lung problems at birth
- Mothers who experience a break in water during pregnancy too early
Signs And Symptoms Of PPHN
The following signs and symptoms may indicate a probability of PPHN (3).
- Fast breathing
- Fast heart rate
- Grunting or moaning while breathing
- Flaring nostrils
- Retraction of the skin between and under the ribs while breathing
- Bluish discoloration of the skin around the lips, hands, and feet (cyanosis)
- Heart murmur
- Low blood oxygen saturation, even when on supplemental oxygen
- Low blood pressure
These symptoms could be similar to other conditions. Therefore, diagnosis is essential to determine the cause.
Diagnosis Of PPHN
The doctor may suspect an anomaly in the baby’s health due to the symptoms. The following diagnostic tests could be conducted to diagnose PPHN (3).
- Chest X-rays to visualize lung issues
- Echocardiogram, a heart ultrasound to check if the baby has any heart problems
- Blood oxygen level assessment through pulse oximetry
- Blood test to check for arterial blood gas level
The doctor may also order other blood tests (cell count and infection markers) and lumbar puncture (spinal tap). These tests may be conducted to rule out other problems or further confirm the presence of PPHN.
Treatment ForPPHN
The goal of the treatment is to increase oxygen supply to all of the baby’s organ systems. The baby might have long-term health problems if their body does not get enough oxygen.
The treatment plan depends on the baby’s symptoms, age, and overall health. It also depends on the severity of the condition. The treatment of PPHNmay include the following (4) (5).
1. Supplemental oxygen
The baby is administered supplemental oxygen in the following ways.
- Endotracheal tube: It is the most efficient way to provide the child with supplemental oxygen. A tube is put in the baby’s trachea (windpipe).
- CPAP (continuous positive airway pressure): This machine gently pushes oxygen into the baby’s lungs.
- Mechanical breathing machine (ventilator): The machine breathes for the baby when the baby cannot breathe.(usually after an endotracheal tube has been insterted)
- High-frequency oscillation ventilation: This special type of ventilator delivers oxygen through rapid, short bursts of air via a breathing tube.
2. Medications
The following medicines are used to treat PPHN and associated disorders.
- Blood pressure medicines might be prescribed to keep blood pressure in check.
- Antibiotics are prescribed to treat and prevent any infection.
- The baby is administered surfactants via breathing tubes to enable their lungs to exchange oxygen and carbon dioxide better.
- Nitric oxide is given to the baby as it helps in expanding the blood vessels in the lungs.
3. Extracorporeal membrane oxygenation (ECMO)
ECMO therapy is done when the baby does not respond to other modes of treatment. In ECMO, the baby’s blood is pumped through artificial lungs outside the body. This artificial lung oxygenates the blood and removes carbon dioxide. The oxygenated blood is then sent back to the baby’s body. This procedure is done under special care in some NICU facilities.
The doctor may consider one or multiple treatments depending on the baby’s symptoms and response to treatment. The baby’s lungs may take weeks or even months to recover fully after the treatment.
Can A Baby Outgrow Pulmonary Hypertension?
Some babies may respond well to treatment and show recovery, although they may not have optimum lung function. According to the American Academy of Pediatrics, some children may eventually require lung or heart transplant (6). However, with the latest advancements in medical science, new treatments are available to prevent the disease from progressing and the baby’s condition deteriorating.
Frequently Asked Questions
1. Can babies survive PPHN?
Chances of survival are 10 to 50% for babies with PPHN, even if it is diagnosed within 72 hours after birth. More than half of the newborns requiring chest tubes for pneumothorax can develop PPHN (7).
2. How long does it take to recover from PPHN?
It may take weeks or months to recover the lung function in babies after PPHN treatment. You may protect your baby from respiratory illnesses such as cold or flu during recovery to avoid complications (8).
3. Is PPHN life-threatening?
Although rare, PPHN can be a life-threatening condition in full-term and post-term babies. Birth complications such as infection and asphyxia can be associated with poor prognosis (3).
4. Is pulmonary hypertension common in newborns?
Approximately two in 1000 live-born term infants can develop severe PPHN. Pulmonary hypertension can be complicated by respiratory failure in more than 10% of newborns (9).
Babies with PPHN may require long-term care even when their condition improves. It is essential to protect the baby from catching the common cold and seasonal flu. Good hand hygiene and avoiding large crowds can help in avoiding these infections. In addition, it is essential to get the baby’s health checkup done regularly and get them screened for normal developmental milestones.
Key Pointers
- A difficult birth, maternal use of NSAIDs, maternal infections such as streptococcal infections, etc., may increase the risk of developing PPHN.
- Fast breathing, rapid heart rate, flaring nostrils, skin retraction between ribs, etc., are some signs and symptoms of PPHN.
- While some babies respond well to treatment, others may need a lung or heart transplant.
References
- Persistent Pulmonary Hypertension in the Newborn.
https://www.stanfordchildrens.org/en/topic/default?id=persistent-pulmonary-hypertension-90-P02400 - Persistent Pulmonary Hypertension of the Newborn (PPHN).
https://www.gosh.nhs.uk/conditions-and-treatments/conditions-we-treat/persistent-pulmonary-hypertension-newborn-pphn/ - Persistent pulmonary hypertension of the newborn (PPHN).
https://www.ucsfbenioffchildrens.org/conditions/persistent-pulmonary-hypertension-of-the-newborn-pphn - Persistent Pulmonary Hypertension of the Newborn (PPHN).
https://www.nationwidechildrens.org/conditions/persistent-pulmonary-hypertension-of-the-newborn-pphn - Persistent Pulmonary Hypertension in the Neonate (PPHN).
https://my.clevelandclinic.org/health/diseases/16020-persistent-pulmonary-hypertension-in-the-neonate-pphn - Pulmonary Hypertension in Infants & Children.
https://www.healthychildren.org/English/health-issues/conditions/heart/Pages/Pulmonary-Hypertension-in-Infants-Children.aspx - PPHN.
https://www.birthinjuryhelpcenter.org/pphn.html#:~:text=Even%20if%20a%20diagnosis%20ofa%20chest%20tube%20develop%20PPHN - Persistent Pulmonary Hypertension of the Neonate (PPHN).
https://www.brighamandwomens.org/assets/BWH/pediatric-newborn-medicine/pdfs/pphn-parentsheet.pdf - Robin H. Steinhorn; 2010; Neonatal Pulmonary Hypertension.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2843001/#:~:text=Severe%20PPHN%20is%20estimated%20toall%20neonates%20with%20respiratory%20failure

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Elna Gibson