Causes Of Prader Willi Syndrome In Babies & Its Symptoms
Babies with PWS display a change in eating, sleeping, and behavioral patterns.
In This Article
Prader Willi syndrome in babies (PWS) is a hereditary condition. It is characterized by symptoms such as small stature, small hands and feet, atypical growth, very low lean body mass, early-onset juvenile obesity, and mild to moderate intellectual and behavioral impairments.

It affects babies of all races and ethnicities and both boys and girls alike. It is also the most frequent genetic cause of life-threatening childhood obesity.
Read on to know the symptoms, causes, complications, diagnosis, management options, and prevention of PWS.
Causes Of PWS In Babies
PWS primarily occurs due to the absence or loss of specific genes in chromosome 15. This abnormality can occur in three ways (1) (2).
- Deletion: This occurs when the chromosome 15 received from the father has missing or deleted critical genes. This occurs in most cases, up to 70%, and is not easily detected during amniocentesis or routine genetic analysis.
- Uniparental disomy (UPD): In up to 30% of PWS cases, the baby inherits two chromosome 15s from the mother and none from the father.
- Imprinting defect/mutation: In 1 to 3% of the cases, a genetic mutation in chromosome 15 inherited from the father causes the genetic material to be inactive despite being present.
The genetic defect in chromosome 15 ultimately affects the normal functions of the hypothalamus, an endocrine gland, which is part of the brain. It is not fully understood why any defects in certain genes of chromosome 15 specifically affect the hypothalamus.
Symptoms Of Prader-Willi Syndrome
The symptoms of PWS appear due to hypothalamic dysfunction. The hypothalamus is responsible for crucial body functions, such as regulating hunger, pain, body temperature, circadian rhythm, fluid balance, and fertility.
The signs and symptoms mostly arise in functions or processes regulated by the hypothalamus. Below are the various signs and symptoms of PWS that could arise over time (3).
- Food craving and weight gain: It is a classic symptom of PWS, usually emerging around the age of two years. Affected toddlers eat large portions and show abnormal food-seeking behavior, such as hoarding, eating raw frozen food, or seeking food in the garbage. The body’s metabolism is slow, too. It can lead to morbid obesity and rapid weight gain, increasing the risk of type 2 diabetes and high blood pressure.
- Poor muscle tone: Hypotonia or poor muscle tone is a common sign of PWS in infants. The babies are small, floppy, and their elbows and knees are loosely rested.
- Sleep disorder: Babies with PWS may experience sleep disorders or disturbances, including sleep apnea. It can lead to excessive sleepiness during the day and may even lead to behavioral issues in older babies.
- Poor sucking reflex: The poor muscle tone causes a poor sucking reflex. It makes it difficult for the baby to latch to the breast or bottle nipple.
- Speech problem: Speech dyspraxia (difficulty in speaking or articulating words) in older babies and toddlers could indicate PWS. Also, babies with PWS may have delayed speech onset.
- Behavioral problems: Older babies and toddlers with PWS may show excessive stubbornness and anger. They may also show symptoms of obsessive-compulsive disorder and pick their skin often.
- Cognitive impairment: Babes with PWS may display learning disabilities and low IQ scores later in childhood. Some other problems include trouble in thinking, reasoning, and problem-solving.
- Distinct facial features: Babies may be born with thin upper lips, turned-down mouth, narrow head at the temple, and almond-shaped eyes.
- Delayed motor development: Children with PWS attain their physical development milestones, such as sitting, crawling, and walking, later than other babies.
- Poor responsiveness: Babies with PWS usually display poor responses to stimuli. They may have weak cries, poor responses to stimuli, or difficulty in waking up.
- Underdeveloped genitals: Girls may have small labia and clitoris, while boys may have small penis and scrotum. Some baby boys may also have undescended testicles. Children with PWS may also experience delayed onset of puberty later in childhood, increasing the risk of infertility during adulthood.
Some other symptoms may include small hands and feet, short stature, scoliosis (curvature of the spine), and high pain tolerance. The symptoms may vary and change in their intensity or visibility as the baby grows older.
Complications Of PWS In Babies
Prader-Willi syndrome may result in the following complications (4).
- Obesity-related complications: These could include type 2 diabetes, sleep apnea, high blood pressure, high cholesterol, and increased risk of gallbladder stones.
- Complications due to inadequate hormone production: Hormone-related complications may include sterility and poor bone health due to inadequate growth hormones. It may eventually lead to osteoporosis, making bones brittle and susceptible to fractures.
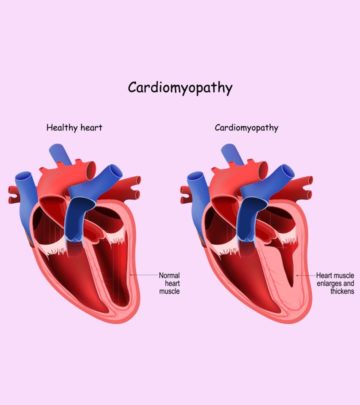
- Physiological complications: These may include heart, joints, muscles, and pulmonary (lung-related) problems.
How Is PWS Diagnosed?
PWS may be diagnosed at birth if the baby displays signs of it, such as low muscle tone and abnormal facial features; there can be a history of feeding difficulty or nasogastric feeding during neonatal period. The doctor may assess the presence of the problem in subsequent checkups as the baby’s insatiable appetite and increased body fat content become apparent.
Blood tests could confirm the presence of genetic abnormalities. Routine genetic tests, such as karyotyping, may not detect this syndrome. DNA methylation analysis is the initial test to identify PWS and does so with greater than 99% accuracy. This test can detect all three forms of PWS (1).
Treatment Of PWS In Babies
There is no cure for Prader-Willi syndrome. However, an early diagnosis of the syndrome and effective management of the symptoms can help improve the child’s quality of life. The doctor can design a specialized treatment that can be modified based on the child’s symptoms and their intensity.
The main objective of treatment and management is to avoid obesity and improve the quality of life. Below are some treatment options that could be considered during infancy and throughout childhood (5) (6).
- Limiting calorie intake and regulating the food served to the baby could help avoid excess weight gain. As the baby grows older, they could be prescribed a specialized diet plan. Other management steps could include encouraging physical activity and controlling the child’s environment to prevent overeating.
- Growth hormone treatment may be suggested by the doctor to improve height, lower body fat, improve muscle mass, and increase bone density.
- Sex hormone treatment may be suggested during early teens if the child does not show the normal onset of puberty.
- Speech and behavioral therapy could be suggested to improve the child’s demeanor and social skills. It could be especially useful if they have behavioral problems, such as obsessive-compulsive disorder.
Prognosis Of Prader-Willi Syndrome
Timely initiation of appropriate treatment steps can improve the child’s quality of life. It can also help individuals with PWS have a normal lifespan. Children could need the right type of education according to their IQ. They will also need speech, occupational, and physical therapies to improve the quality of life (4).
Prevention Of Prader-Willi Syndrome
There is no way to prevent Prader-Willi syndrome since it is a genetic disorder. Adequate prenatal care and healthy habits, such as eating a healthy diet and avoiding tobacco and alcohol, may help reduce the risk of genetic defects in general. PWS may run in families. If you have a family history of the disorder or already have a child with the condition, speak to a genetic counselor before planning your pregnancy.
Frequently Asked Questions
1. Can Prader-Willi syndrome be fatal?
Prader-Willi syndrome is not fatal in itself. However, the symptoms of the condition, such as compulsive eating, may cause the onset of severe conditions, such as type 2 diabetes, later in life (7).
2. Is Prader-Willi syndrome detected before birth?
Yes, it is possible to detect Prader-Willi syndrome before birth via noninvasive prenatal testing (NIPT) or cell-free DNA testing. You can do this test anytime after nine or ten weeks of pregnancy (8).
Prader Willi syndrome in babies is caused by abnormalities in chromosome 15. The disorder primarily affects a child’s metabolism, physical appearance, and behavior. Further, hypothalamic dysfunction affects their eating patterns and metabolism, resulting in weight gain and poor muscle tone. Slow cognitive and motor developments are also some symptoms of the syndrome. In addition, babies with Prader Willi syndrome may face complications due to obesity, hormonal imbalance, and improper functioning of the heart and lungs. However, early diagnosis and management, including diet plans, hormone treatment, and behavioral therapies, can improve the baby’s quality of life.
Key Pointers
- Prader Willi syndrome (PWS) follows a hereditary nature and is caused due to a genetic deletion on the 15th chromosome.
- Delayed growth and motor skill development, decreased muscle tone, behavioral and speech issues are classic signs of PWS in babies.
- Contact a pediatrician to confirm it with an appropriate diagnostic method.
- To know some effective treatment options, scroll down.
References
2. What Is Prader-Willi Syndrome?; Prader-Willi Syndrome Association
3. Prader-Willi syndrome; University of Florida
4. Prader-Willi Syndrome; Cleveland Clinic
5. Diagnosis & Treatment- Prader-Willi Syndrome; Foundation for Prader-Willi Research
6. Prader-Willi Syndrome; National Organization for Rare Disorders
7. Overview: Prader-Willi syndrome; NHS
8. Noninvasive Prenatal Screening – Testing Now Available For PWS; Prader Willi Syndrome Association, USA

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Rana Chanchal