Thrombocytopenia In Pregnancy: Causes, Risks And Treatment
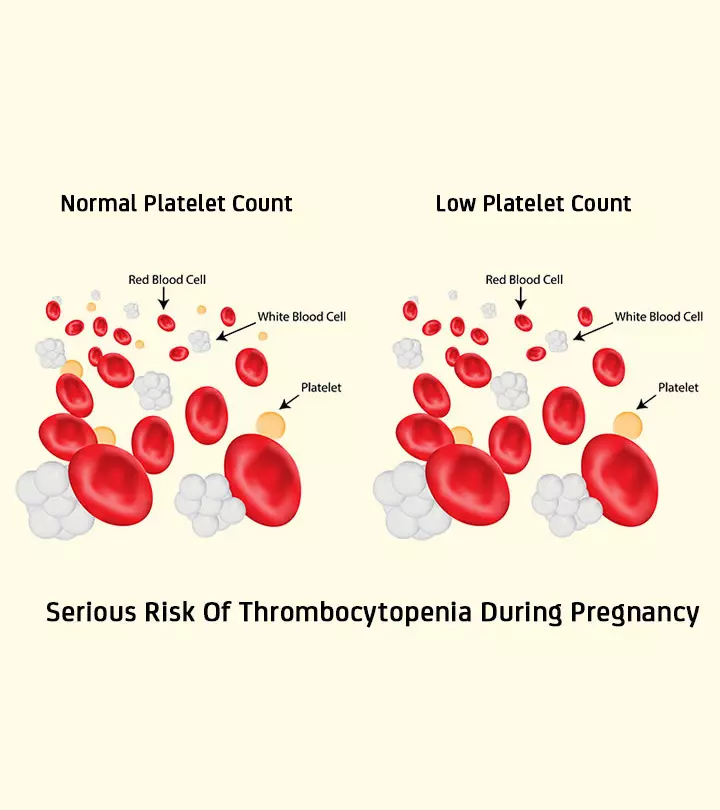
Image: Shutterstock
In This Article
Thrombocytopenia (low platelet count) is a common blood disorder in pregnancy. It could result from pregnancy-specific conditions or due to other reasons.
In this post, MomJunction tells you about the various conditions that cause thrombocytopenia during pregnancy, its treatment and natural ways to improve the platelet count.
What Is Thrombocytopenia?
Thrombocytopenia is a persistent decrease in platelet count. The normal count ranges from 150,000 to 400,000 platelets per microliter (µl) of blood. A drop in platelet count to below 150,000 platelets per µl is known as thrombocytopenia (1).
A slight drop is not a matter of concern as it does not cause any complication for the mother or the baby. However, an extreme decrease in the platelets could lead to complications and needs medical attention.
How Common Is Thrombocytopenia During Pregnancy?
Thrombocytopenia is the second most common blood disorder during pregnancy, after anemia. It is known to occur in 8 – 10% of all pregnancies (2). The condition is classified based on the severity of the decline in the platelet count.
Classification Of Thrombocytopenia
The severity of thrombocytopenia is classified as below:
- Mild thrombocytopenia: >100,000
- Moderate: 50,000 -100,000
- Severe: <50,000
During pregnancy, most thrombocytopenia cases are mild but if the platelet count is less than 80,000, you need to consult the doctor (3).
What Are The Causes Of Thrombocytopenia In Pregnancy?
It most commonly happens due to decreased platelet production or increased platelet destruction. The most common causes of thrombocytopenia during pregnancy are:
- Gestational thrombocytopenia (75% of all thrombocytopenia cases in pregnancy)
- Preeclampsia and HELLP syndrome (15-20%)
- Immune thrombocytopenic purpura (3%)
- Others (8%)
Let us see each of them in detail:
1. Gestational thrombocytopenia (GT)
This is also known as incidental thrombocytopenia and develops in about 4.4%-11.6% of all pregnancies (4). It is associated with increased platelet activation and increased peripheral consumption of platelets because of their reduced lifespan in pregnancy.
The characteristics of gestational thrombocytopenia are:
- There are generally no symptoms.
- The condition is mild to moderate with a platelet count of more than 70,000 per µl.
- It mostly develops in the third trimester and is usually detected during the routine prenatal screening.
- The platelet count returns to normal within 2 – 12 weeks post pregnancy.
Risks involved:
Gestational thrombocytopenia poses no risks either to the mother, fetus, or neonate (a newborn child). The mother does not require treatment besides periodic monitoring. In some cases, the doctor might suggest periodic monitoring even after the delivery.
2. Immune thrombocytopenic purpura (ITP)
Also known as idiopathic thrombocytopenic purpura or autoimmune thrombocytopenic purpura (ATP) (5), ITP is difficult to distinguish from GT. However, this condition is present even before pregnancy, and the women have a history of abnormal bleeding and low platelet count.
ITP is an autoimmune disorder caused by the development of antiplatelet antibodies.
The characteristics of immune thrombocytopenic purpura are:
- Women can be asymptomatic or have a history of easy bruising, mucosal bleeding, petechiae (purple spots on the skin caused by minor bleeding) and gingival bleeding.
- This condition is present before conception and would continue post delivery.
- It needs close follow-up during and post delivery.
Risks involved:
- In most cases, infants born to women with ITP do not have any symptoms. A few might have a low platelet count but the complications are very rare. However, the platelet count needs to be monitored for several days after birth for any fluctuations.
- Minor bleeding complications in the neonatal period include purpura (purple spots on the skin), melena (dark tarry stools) and ecchymosis (escape of blood from ruptured blood vessels).
- The mother is at the risk of developing spontaneous hemorrhage if the platelet count drops below 20,000/µl.
Treatment is necessary for women with a platelet count below 10,000/µl at any time of pregnancy, or below 30,000/µl in the third trimester.
3. Preeclampsia and HELLP syndrome
Preeclampsia is the second most common reason for thrombocytopenia during pregnancy. It occurs due to high blood pressure during pregnancy and may lead to HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome (6).
The characteristics of HELLP syndrome are:
- The platelet count could be below 100,000/µl.
- It usually develops around the third trimester between 28 and 36 weeks of pregnancy.
- The symptoms of HELLP syndrome include abdominal pain, soreness in the upper right quadrant, and epigastrium.
- Proteinuria and hypertension occur in 85% of the cases.
- Thrombocytopenia is severe in HELLP than in preeclampsia patients.
Risks involved:
- Fetal growth may be restricted.
- Neonates have a risk of developing thrombocytopenia.
- The mother may need platelet transfusion if there is bleeding.
- HELLP syndrome is more common in women giving birth to multiple babies.
HELLP syndrome is a serious condition and requires your doctor’s attention.
Other Causes Of Thrombocytopenia During Pregnancy
Whereas the above three are the most common causes of thrombocytopenia during pregnancy, there are a few other reasons too. We list them below:
4. Thrombotic microangiopathies
Thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) are together referred to as thrombotic microangiopathies. They are characterized by low blood platelet count and hemolytic anemia (7).
The thrombotic microangiopathies are known to occur in one out of 25,000 pregnancies. The incidence is greater in the second and third trimesters. Microangiopathies are usually mistaken for preeclampsia or HELLP syndrome, as the symptoms are similar. TTP affects the central nervous system, and HUS affects the kidneys.
Plasmapheresis (plasma exchange) is the first line of treatment. It removes the platelet aggravating substances that cause TTP and HUS.
5. Acute fatty liver of pregnancy (AFLP)
AFLP is a rare disorder and occurs in one out of 10,000-15,000 pregnancies, mostly in the third trimester or early postpartum period. It is known to occur because of abnormalities in the intramitochondrial fatty acid beta-oxidation (8).
The symptoms include nausea, vomiting, pain in the upper right quadrant, malaise, and cholestatic liver dysfunction (impairment of bile flow).
6. Nutritional deficiencies
Severe deficiency of vitamin B12 and folic acid can cause low platelet count associated with low red and white blood cell counts. However, it is rare in pregnancy as women take folic acid supplements to prevent neural tube deformities. Vitamin B12 deficiency is also uncommon in pregnancy.
7. Medicine-induced
Certain medicines such as paracetamol and ibuprofen that influence the formation of platelets in the blood, also affect platelet production.
The various other causes include:
- Pseudothrombocytopenia
- Disseminated intravascular coagulation (DIC)
- Heparin-induced thrombocytopenia (HIT)
- Type 2B von Willebrand disease
- Marrow infiltrative disorders
- Autoimmune diseases systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS)
- Other inherited thrombocytopenias
- Cancers such as lymphoproliferative syndrome and myelodysplastic syndrome
What Happens If You Have Thrombocytopenia During Pregnancy?
If you have low platelet count before pregnancy or if it is detected in the early stages of pregnancy, it could be due to an underlying condition as mentioned in the previous section or due to any medication. Your doctor will monitor the condition over time to check if the condition is benign.
If the low platelet count is detected in the later stages, your doctor might check for the other signs of preeclampsia or HELLP syndrome.
Treatment For Low Platelet Count During Pregnancy
The treatment depends on the severity of the condition and focuses on addressing the cause. Mild cases do not need any medical treatment but need regular monitoring. Severe causes such as preeclampsia, SLE, HELLP require medical treatments.
The treatments include:
- Corticosteroids may rapidly increase the platelet count and lower the risk of bleeding (9).
- Immunoglobulin injections may increase the platelet count (10).
- Concentrated platelet transfusion immediately improves the condition.
- Rinsing with aminocaproic acid when there is excessive bleeding from the mucus membrane of the mouth.
- If none of the above treatments work, splenectomy (spleen removal) is done during the second trimester (10). However, this surgery is reserved for conditions where platelet destruction is involved.
What Are The Risks Of Low Platelet Count During Pregnancy?
If the platelet count falls during pregnancy, and the suggested treatment doesn’t work, there might be some risks during delivery.
- The uterus has the largest supply of blood vessels; with low platelet count, the blood might not clot resulting in excessive blood loss during delivery.
- The newborn might have internal bleeding.
- Contradiction with the use of epidural as you will be at the risk of epidural hematoma (accidental puncture of the spine) (11).
How to Increase Low Platelet Count Naturally?
The following natural remedies help in increasing the platelet levels in the blood (12).
- Eat colorful fruits and vegetables such as berries, oranges, kiwis, tomatoes and green leafy vegetables. They boost the immune system and raise platelet count.
- Consume freshly made beetroot and carrot juices. They improve platelet levels in the blood.
- Take vitamin C-rich foods such as spinach, lemon, bell pepper, and broccoli. They help in restoring the platelet level.
- Have freshly made gooseberry pickle or jam. It is a blood purifier and helps platelet production.
- Omega-3 fatty acid foods boost immunity and naturally promote platelet levels. Include eggs, fish, flaxseed oil, tuna, and salmon.
- Whole grains contain phytoestrogens and vitamin E that lower the platelet aggregating effect of blood and thus increase the platelet levels.
- Walnuts, cooked carrot, peanuts, black sesame, lean meats, and milk also increase the platelet count.
The exact reason for thrombocytopenia during pregnancy might be difficult to diagnose because of the overlapping pathophysiology. In most cases, it is mild and would not have an effect on the baby, but your doctor will monitor the levels regularly to make sure the count is not too low. When the condition is not severe, have a balanced diet and take care of your health, while keeping a close watch on any unusual symptoms.
Do you have any experience to share? Let us know about it in the comments section below.
References
2. Bethan Myers; Review thrombocytopenia in pregnancy; Royal College of Obstetricians and Gynaecologists (2009)
3. Thrombocytopenia in Pregnancy; NCBI
4. Elmukhtar Habas Sr et al.; Gestational Thrombocytopenia: A Review on Recent Updates; Cureus (2022)
5. Evi Stavrou & Keith R. McCrae; Immune thrombocytopenia in pregnancy; Hematol Oncol Clin North Am (2010)
6. Vigil-De Gracia P; Pregnancy complicated by pre-eclampsia-eclampsia with HELLP syndrome; Int J Gynaecol Obstet (2001)
7. George JN et al.; Syndromes of thrombotic microangiopathy associated with pregnancy; Hematology Am Soc Hematol Educ Program (2015)
8. Hin Hin Ko & Eric Yoshida; Acute fatty liver of pregnancy; Can J Gastroenterol (2006)
9. Selim Kurtoğlu et al.; Fetal adrenal suppression due to maternal corticosteroid use: Case Report; J Clin Res Pediatr Endocrinol (2011)
10. Srividhya Sankaran & Susan E Robinson; Immune thrombocytopenia and pregnancy; Obstet Med (2011)
11. Linden O. Lee et al.; Risk of epidural hematoma after neuraxial techniques in thrombocytopenic parturients: A Report from the Multicenter Perioperative Outcomes Group; Anesthesiology (2018)
12. Swati Burungale; Natural remedies to increase platelet count; The Pharma Innovation Journal (2016)

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.