Asthma In Babies: Causes, Symptoms And Treatment

Image: Shutterstock
Asthma can lead to uncomfortable symptoms in the baby. While it makes breathing difficult, it may also interfere with day-to-day activities. In some cases, children may outgrow it by their teens. Nevertheless, adequate care and support can help child with asthma live a healthy life. So, what causes asthma and can a child outgrow it? We help answer these questions and more about asthma in babies.
In This Article
What Is Asthma?
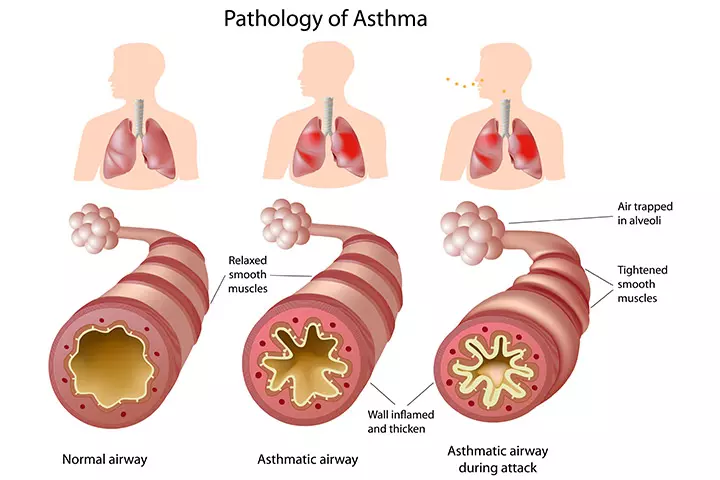
Asthma is a condition where the airways that carry air to the lungs get swollen and inflamed, thus hindering the airflow. The inhaled air passes into parts of the throat such as larynx, eventually entering the trachea, also called the windpipe. The trachea runs towards the lungs where it branches out to bronchi (singular: bronchus). Each bronchus enters the lungs to divide into smaller branches called bronchioles, which end in a sac called alveoli.
In asthma, the lower trachea and bronchi with bronchioles develop a severe inflammation in their inner lining. The swollen tubes constrict the internal space, and it limits the amount of air reaching the lungs. The condition is further worsened by the secretion of surplus mucus by the inner cells and the thickening of the external airway. All these conditions make it difficult to breath, leading to asthma (1).
Let’s see how or what causes the inflammation and blockage.
What Causes Asthma In Babies?
The fundamental cause for asthma is not yet known (2). Experts state that the condition is primarily genetic. It means the disease is a result of a defective gene that can pass from one generation to the next. Asthma is also interrelated to allergies such as eczema, which is also genetic.
Some specific conditions, agents, and events can trigger asthma in babies, who carry the defective gene for asthma. The following are the most common causes of asthma among infants:
- Allergens: Air or food allergens can trigger asthma in an infant. Even dust mites, insect droppings, and fur of animals can be potential allergens.
- Respiratory infections: An infection of the upper respiratory tract, such as the common cold, pneumonia, and flu, can cause inflammation of the airways along with excess mucus secretions. It can precipitate an asthma attack.
- Physical activity: Playing a game or intense activity that requires heavy movement can trigger asthma. Such type of attack is called exercise-induced asthma.
- Air pollutants: Vehicular effluents, tobacco smoke and such pollutants trigger an asthma attack. Also, strong smells and fragrances may also cause asthma. Passive smoking is an important risk factor.
- Cold and dry air: Dry, cold air stimulates the production of mucus, which in the case of an asthma patient may make it difficult to breathe.
- Certain medications: Medicines, which usually come under the category of non-steroidal anti-inflammatory drugs (NSAIDs) (3), act on the immune system and may trigger asthma in an infant, who is susceptible to it. Most of these trigger medicines, except acetaminophen (sold as Tylenol) and ibuprofen (sold as Advil), are usually not prescribed to infants.
- Some food preservatives: Older infants may consume a wide variety of food that could include foods that contain preservatives. Some preservatives may have the potential to trigger a food allergy, which could indirectly cause asthma. One such preservative is sulfate that is often added to dry fruits.
These factors may not lead to asthma in all the babies but some infants are at a higher risk.
What Are The Risk Factors For Asthma In Babies?
According to the American Academy of Pediatrics (AAP), the following factors play a crucial role in determining if a baby would develop asthma (4):
- Parents have asthma: Since the condition is mostly genetic, if a parent has asthma, then there is a high probability of the baby developing the condition.. Having a close relative with asthma can also increase the risk.
- Presence of eczema: Research has noted that both eczema (also called atopic dermatitis) and asthma are the results of the same mutated gene (5). Therefore, there is a high correlation between the two conditions. In fact, about 20% individuals with eczema also develop asthma (6).
- Allergies towards air allergens: Allergies towards airborne substances and asthma are interrelated. About 60% of individuals with asthma have allergic asthma (7). Allergy occurs when the immune system mistakenly detects a foreign substance as a pathogen and mounts an attack on it. Common air allergens are pollen, dust mites, plant fibers, molds, and fungal spores. When a baby inhales any of these allergens, the immune system cells secrete a complex chemical called immunoglobulin E (IgE). IgE leads to airway inflammation and accelerated mucus secretion, which eventually trigger asthma.
- Food allergies: They also lead to the secretion of IgE, which may affect airways to cause asthma attacks. Asthma due to food allergies is quite rare, although it does exist (8).
- High eosinophil count: Eosinophils are a type of white blood cells that are often noted in higher numbers when someone is prone to allergies. A baby with greater than 4% eosinophil concentration in the blood and saliva can be susceptible to developing asthma (9).
- Wheezing during cold: If a baby tends to wheeze every time they get cold, then their airways could be chronically constricted. This may make them vulnerable to asthma.
Asthma can occur in newborns and in infants that are being breastfed (10). Learning the signs of asthma in babies is vital to tackle the condition efficiently.
What Are The Symptoms Of Asthma In Babies?
According to the Asthma and Allergy Foundation of America (AAFA), a baby with asthma will display the following symptoms (11):
- Fast breathing: The baby would breathe in and out rapidly with shorter gaps between breaths. On an average, an infant makes 30 to 60 breaths per minute until the age of three months. From three to 12 months it would be between 20 to 40 breaths. Asthma causes a 50% increase in the number of breaths made by the infant.
- Strain during breathing: The infant has to work harder at getting air into their lungs. And, the strained breathing is visible through flared nostrils, an inward press of the ribs, and excessive belly movement.
- Chest tightness: Every time you touch the baby’s chest, you find it stiff. It is because the thoracic muscles are always taut due to shortness of breath.
- Wheezing: The whistling sounds occur during breathing and are quite likely due to strained breathing.
- Chronic cough: This most likely happens during the night or while outdoors.
- Huffing and panting: They are caused due to severe shortness of breath during activities involving physical effort such as crawling and walking with support.
- Softer crying sound: Young infants and newborns would make feeble sounds while crying due to their inability to breathe properly.
- Lethargy and constant tiredness: These are characteristic of asthma.
- Pale or blue coloring on the face and hands: This occurs around lips and nailbeds of hand, and is a sign of low levels of oxygen in the blood (12).
In the case of an asthma attack, the baby experiences same symptoms, but with higher intensity.
What Is An Asthma Attack In Babies?
Asthma attack displays the usual symptoms of asthma – shortness of breath, rapid breathing, and wheezing, but with substantially greater severity. Depending on the intensity, asthma attack is categorized into the following scales (13):
Mild asthma attack: Shortness of breath happens only while crawling or walking. The baby is able to cry or babble normally without any difficulties. Mild wheezing might exists.
Moderate asthma attack: Shortness of breath and wheezing happen even when the infant is at rest. The baby is unable to babble due to insufficient breath. The wheezing is audible, and you can also see the chest retracting with each breath, indicating difficulty in breathing.
Severe asthma attack: The shortness of breath is extreme even at rest, and the wheezing is so frequent that it is quite loudly audible. The infant is unable to get air into the lungs and would struggle to breathe despite gasping for air.
If your baby is having an asthma attack, then see a doctor immediately.
What To Do When A Baby Has An Asthma Attack?
Give the baby a dose of quick-relief medicine through a metered dose inhaler (MDI). The metered dose inhaler, also called an asthma pump, is the primary first aid for asthma in babies. Once your baby’s asthma has subsided, take them to a doctor right away.
Usually, parents are provided an asthma action plan by the doctor if the infant has clinically-diagnosed asthma (14). The asthma action plan contains instructions about the medicines to be administered during an attack. Parents are also instructed to maintain a written record of the date, time, and intensity of the attack. The steps and instructions in the asthma action plan would vary depending on the baby’s age and severity of the condition (15).
How Is Asthma In Babies Diagnosed?
There is no single test to detect asthma in babies (16). A doctor will use the following steps to diagnose asthma:
- Learn about the baby’s symptoms: The doctor learns the baby’s symptoms from the parents, who are also asked about the situations when the baby shows symptoms..
- Review the infant and family’s medical history: You need to be honest with the physician about the family history of asthma, allergies, and eczema, or about baby’s current allergies. It significantly helps improve the accuracy of diagnosis.
- Chest X-rays: They determine any blockage in the bronchioles that could indicate swelling of the tissue and the accumulation of mucus.
- Blood test: They find the eosinophil number. A high count of eosinophil can be an indicator of asthma.
The information collected through the above procedures helps the pediatrician arrive at a definite diagnosis of asthma.
How To Treat Asthma In Babies?
There is no cure for asthma. Reducing the frequency of the symptoms and preventing asthma attacks is the only way to manage the condition (17). The “treatment” of asthma aims at long-term management of the condition, and there are several modes of delivery of asthma medicines.
Modes of asthma medicine delivery:
The following equipment and procedures are used to administer asthma medication to an infant (18):
- A nebulizer is a machine about the size of a small box. A liquid medicine is poured into a slot within the machine. The device evaporates the liquid into a mist that flows through a tube, which ends in a mask worn by the infant around nose and mouth. A nebulizer is the most preferred choice for asthma medicine delivery in infants as it is easy for a parent to administer (19).
- A metered-dose inhaler (MDI) is also called asthma pumps. They give out a small dosage of medicine and require pumping and breathing the medicine at the same time. MDIs are always used with spacers for infants with asthma. Spacers are large plastic tubes that often contain a mask, which can be securely strapped to the baby’s face. The MDI pump is attached at the end of the spacer tube. When the pump is pressed, the medicine releases within the spacer tube and goes straight into the infant’s mouth and then to the lungs. It ensures that the baby gets all the medicine without wastage (20).
- A dry powder inhaler (DPI), also called as a diskus as the device resembles a small disc, delivers medicines in dry powder form. Powder-filled capsules are loaded manually within the diskus. Alternatively, it can be a sealed diskus with powder within, and the device has to be replaced with a new one after the powder is exhausted. DPIs are used like MDIs but without a mask. The mouthpiece of diskus is inserted into the mouth and a button is pressed. It releases the powder with pressure making it land straight into the windpipe from where it reaches the bronchioles and lungs.
- Only a few medicines are used for injections, usually in the cases when asthma is the result of an underlying allergy. However, the first choice of treatment is MDIs and nebulizer. But if the infant shows no improvement, then the doctor may consider tackling the allergy through injectable medicines or syrups that act directly on the immune system and suppress its allergies (21).
Medicines for asthma treatment:
There are fundamentally three types of medications used in the treatment of asthma – long-term control medicines, quick-relief medicines, and medicines for allergy-induced asthma. There are several drugs within each category.
i) Long-term control medicines
These are medicines used for long-term management of asthma, and the infant takes them daily to prevent asthma symptoms efficiently. The severity and prognosis of asthma after infancy will determine if the infant needs to have controller medicines for long term. The following are the commonly used control medicines for babies:
- Inhaled corticosteroids: Corticosteroids help reduce the inflammation of the inner lining of the bronchioles. Corticosteroids are the first choice of controller medicines for infants since they have minimal side effects and can be used daily. The nebulizer is the preferred mode of delivery for inhaled corticosteroids while MDI can be used as well.
- Long-acting beta agonists: These are chemical substances that dilate the external smooth muscles of the bronchioles (22). It significantly relaxes the airways thus making breathing easier. Long-acting beta agonists are ONLY administered in combination with corticosteroids as beta agonists alone have detrimental side effects such as reduction in lung efficiency (23) (24). Several corticosteroid medications may contain some beta agonists and are thus called combination medicines. Nevertheless, beta agonists are given to infants only if they display no improvement with corticosteroids alone.
ii) Quick-relief medications
The medicines are also called rescue asthma medicines and are either delivered through MDI or intravenously. Quick-relief medication provides instant relief from wheezing, breathlessness, and tightness in the chest muscles. They are not a long-term solution and only aim at giving immediate improvement and relief from an asthma attack. The following are the commonly used quick-relief asthma medicines:
- Short-acting beta agonists: These are related to long-acting beta agonists, but act faster with a limited duration effect. Short-acting beta agonists are administered immediately during an asthma attack using a nebulizer or an MDI. These drugs can have side effects when used long-term. Therefore, they are only recommended for immediate recovery from an asthma attack (25).
- Ipratropium: It is a medicinal compound used for making breathing easier in bronchitis, but it is also effective against asthma attacks. The medicine is a bronchodilator and relaxes the smooth muscle fibers on the bronchioles. Long-term usage of the medicine has side effects thus it is only prescribed for use during asthma attacks (26).
- Intravenous corticosteroids: Unlike inhaled corticosteroids, intravenously administered corticosteroids provide short-term relief and are only used in cases of severe asthma attacks. The medicine is considered as a last resort for an asthma attack and is seldom given to infants.
iii) Medicines for allergy-induced asthma
If asthma is always triggered by allergies or if the infant has a severe asthma attack every time he is exposed to a potential allergen, then the baby will need some specialized medicines. Medication for allergy-induced asthma works in conjunction with long-term control treatment and the quick-relief medicines. Here is what is used to treat allergy-induced asthma:
- Allergy shots: It is a course of intravenous medications that bring down the sensitivity of the immune system towards potential allergens. This treatment is also called immunotherapy. The baby gets an injection once a week for a few months depending on the intensity of allergy. Later, the frequency of dosage could be reduced to one injection per month for three to five years.
- Omalizumab: It is a compound that lowers the hypersensitivity towards an allergen by altering the quantity of immunoglobulin E (IgE) secreted by the immune system (27). High IgE level is an indicator of severe allergy and allergies can cause asthma. Administering omalizumab reduces the quantity IgE thus providing relief from asthma.
A combination of the above treatment procedures helps the baby live a better life with asthma. However, managing asthma at home is equally important and vital to prevent the likely onset of asthma symptoms.
How To Prevent Asthma In Babies?
There is no specific way to prevent asthma (28). But, the potential triggers can be kept at bay. Here is what you can do:
- Clean and vacuum your baby’s room every day to prevent accumulation of dust, mites, and pollen.
- Wash baby’s bedding every week in warm water of 130°F (54°C). If your baby is severely allergic, then it is advisable to wash the baby’s clothes also in warm water.
- Only buy washable toys and wash plush soft toys weekly with warm water.
- Keep the baby away from pets. Dry skin from pets, called dander, and pet fur can induce an asthma attack.
- Use an air purifier that has high-efficiency particulate air (HEPA) filter, which filters out the microscopic particulate matter in the air. Alternatively, use a fine-net window mesh that will help keep dust, pollen, mites and tiny insects out.
- Use a humidifier as it adds humidity to ambient air, making it easy for a baby to breathe during dry conditions. The AAP recommends the use of only cool-mist humidifiers for a baby’s room since they do not pose a risk of burns unlike hot-mist/steam humidifiers (29).
- Keep the baby away from tobacco smoke and vehicular effluents. Do not let anyone in the house smoke around the baby. When going outdoors, keep the baby away from vehicular effluents.
- Avoid foods that trigger an allergy in the baby. Give fresh, home-cooked food to such infants.
Do not use any essential oils for inhalation to treat or subdue the infant’s asthma symptoms as it may accidentally aggravate the condition (30). Manage asthma with the above home remedies and consult a doctor to get additional information. Asthma in infants is a complex condition and parents are bound to have a few more questions, which we answer in the next section.
Frequently Asked Questions:
1. Can my baby outgrow asthma?
Probably. About 50% infants stop having asthma symptoms once they reach adolescence. But some experts believe that infants do not exactly outgrow asthma, instead display fewer symptoms as they grow older. The tolerance also improves as one grows older and manages the disease better.
2. What are the foods to avoid for a baby’s asthma?
The common foods associated with food allergies are:
- Nuts (including nut-based foods such as peanut butter)
- Fish (including shellfish)
- Wheat and wheat products (crackers and bread)
- Dairy products (made with cow or buffalo milk)
- Eggs
- Soybean
Experts state that there is no evidence that avoiding potential food allergens can prevent asthma in infants (31). Some of the above food items are a vital source of nutrients for older infants. Consult the doctor if you suspect a food item to be an allergen or intend to discontinue it to mitigate the chances of asthma.
3. Can asthma resemble the symptoms of other diseases?
Yes. Some diseases have symptoms such as wheezing, shortness of breath, and chest tightness that resemble asthma. Examples are:
- Croup
- Pneumonia
- Epiglottitis
- Bronchitis
- Bronchiectasis
Remember, these diseases present other symptoms that are absent in asthma. Also, their prognosis is significantly different from that of asthma.
4. Does baby powder cause asthma?
Yes. Baby powder or any talcum powder can trigger asthma in a baby, who already has the condition. Pediatric experts recommend against the use of baby powder for babies with asthma (32).
5. Can swimming cause asthma in babies?
There is no conclusive evidence on it. Several research studies have produced conflicting results. A study by the AAP found that swimming does not directly increase the risk of asthma in infants. Instead, there is an increase of upper respiratory tract infections that could lead to asthma (33). The risk occurs due to chlorine, which is commonly added to swimming pool water for disinfection. Chlorine dissolves from water to the air above the pool from where a baby inhales it. The chlorine may cause damage to the baby’s delicate airways thus increasing the risk of infections, which can indirectly lead to asthma.
Most experts state that there is no definite link between asthma and chlorinated pools (34). If you intend to let your baby swim, then opt for baby-friendly pools that do not add any chemicals to the water. Choose outdoor pools where the chlorine can dissipate. When selecting indoor pools, choose facilities that have adequate ventilation to prevent a buildup of chlorine in the air.
6. Can acid reflux cause asthma?
No evidence points towards acid reflux, that is, gastroesophageal disease (GERD) as a direct cause of asthma. However, the two conditions can influence each other’s intensity. About 75% individuals with asthma also experience GERD (35). The exact relation between the two diseases is unknown, but there are two hypotheses. One is that if a person has GERD, then the repeated reflux could cause refluxed stomach acid to trickle into the airways where they can inflame the inner lining and cause asthma. Another conjecture is that reflux causes a nerve trigger in the upper respiratory system causing the person to cough and splutter, which in long-term could cause asthma. On the flip side, some asthma medicines trigger GERD as a side effect. Nevertheless, there is no conclusive evidence about the relation between the two (36).
7. Do all pets cause asthma in babies?
Mostly furry and feathered animals tend to be allergenic. Cats are more likely to trigger asthma than dogs. However, it is not fur alone that can trigger asthma, but also flakes of dead skin (dander) that fall from these pet’s skin. Feathers from birds is also a trigger (37). About 30% individuals with asthma have an allergy towards pets. Pets that usually do not trigger asthma are fish, reptiles, and amphibians. Most asthma experts recommend choosing these animals over furry ones if you intend to have a pet and live with a baby with asthma (38).
8. Can smoking during pregnancy cause asthma in babies?
Yes. There is strong evidence that babies born to women who smoke during pregnancy are at a higher risk of having asthma. The infant will also be four times more likely to have life-threatening asthma attacks than babies with asthma whose mothers did not smoke during pregnancy (39).
9. Are C-section babies at a higher risk of asthma?
C-section babies do seem to display a higher incidence of developing asthma than infants who have a vaginal birth. Experts note that birth through the birth canal rubs specialized bacteria onto the baby, offering them protection against diseases such as asthma. It is to be noted that C-section born infants are just more vulnerable than their naturally-born peers but does not mean that all C-section infants will develop asthma (40).
10. Can asthma happen in premature babies?
Yes. Preterm infants are at a higher risk of developing asthma later in life. The primary reasons are the underdeveloped airways at birth and the baby’s susceptibility toward upper respiratory tract infections that lead to asthma (41). Nevertheless, precautions and care can help prevent the condition in preterm infants.
Remember that asthma need not be a hindrance to growth. An infant can continue to grow the healthy way and reach all their developmental milestones if you manage the condition well. Proper care is the key to help a baby with asthma live a life without limits.

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Rohit Garoo