Spina Bifida In Babies: Types, Symptoms, Diagnosis & Treatment
The symptoms are often visible right at birth, letting initiation of treatment.
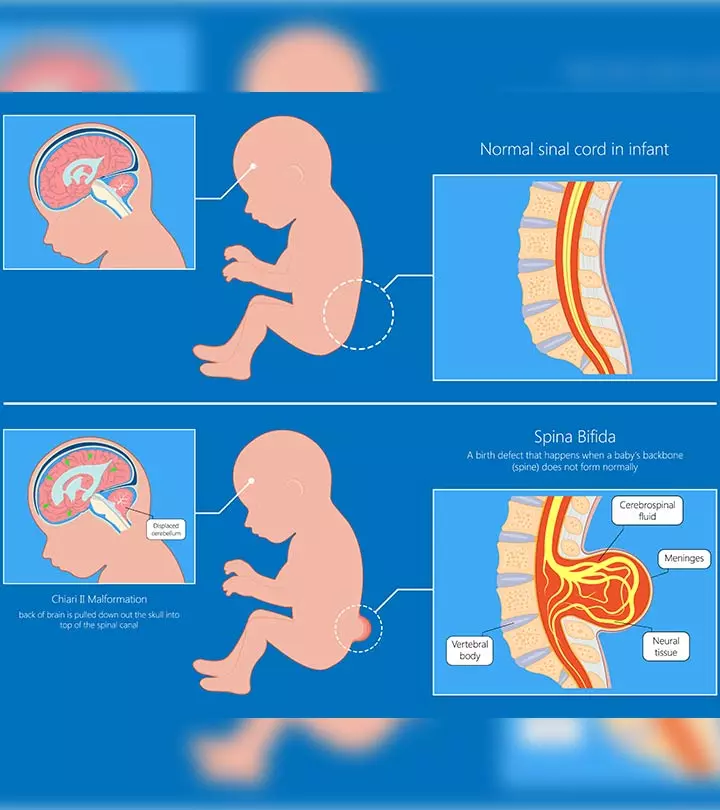
Image: Shutterstock
In This Article
Spina bifida in babies is the most common neural tube defect, which can impair your toddler’s brain, spine, spinal cord, and meninges (tissues covering and protecting the brain and the spinal cord). The term “spina bifida” refers to a “split spine” or “open spine” (1). that develops when the vertebral column (spinal cord bones) are not formed correctly, resulting in a gap or opening. It can happen anywhere along the spine’s length.
Read on to know about the forms and causes of spina bifida and how it can be diagnosed, treated, and prevented in babies.
Types Of Spina Bifida
The following are the different types of spina bifida in babies (2).
1. Spina bifida occulta
- It is also known as hidden spina bifida, and it is the mildest and commonest form of the condition.
- It does not usually cause any health problems and may go undiagnosed.
- There is a gap in the spine, but it is too small to cause any impact on the spinal cord and nerves.
- A dimple, hairy patch, dark spot, or swelling may be seen on the skin over the gap.
2. Meningocele
- It is the rarest form.
- The meninges push out through a gap in the spine and cause the formation of a fluid-filled sack called meningocele on the baby’s back.
- The sack does not have any portions of the spinal cord.
- There is little or no impact on nerves.
- Some babies might have problems controlling bladder and bowel movements due to the meningocele.
- The meningocele can be surgically removed.
3. Myelomeningocele
- It is also called open spina bifida, and it is the most severe form of spina bifida
- A part of the spinal cord pushes out along with the meninges through the opening in the spine and forms a fluid-filled sac on the baby’s back.
- It may cause damage to the spinal cord and nearby nerves.
- It may lead to moderate to severe disabilities or paralysis in severe cases.
- It may lead to life-threatening infections in some cases.
- It may lead to problems with how the baby uses the bathroom, loss of sensation in the legs or feet, or inability to move legs.
4. Closed neural tube defects
- In this type of defect, there are problems with the formation of fat, bone, or meninges around the spinal cord.
- It may lead to nerve damage in the spinal cord.
- It does not usually cause any symptoms, but it may lead to bladder and bowel control problems in some cases.
Risk Factors And Prevention Of Spina Bifida In Babies
According to the Centers for Disease Control and Prevention, the exact causes of spina bifida are unknown (2). However, the following are the identified risk factors that may be avoided to prevent spina bifida in babies.
- Folic acid: Inadequate maternal folic acid consumption during pregnancy may lead to birth defects, including spina bifida. Supplementation of folic acid during and before pregnancy may help prevent spina bifida and other neural tube defects.
- Genes: Genetic factors may cause spina bifida. However, more research is needed to establish a relationship between genetic causes and spina bifida. Mothers who have had a baby with spina bifida have a four percent risk of having another baby with spina bifida (3). Parents with neural tube defects are at a higher risk of having babies with spina bifida. If you or anyone in your family has a baby with spina bifida, you must consider visiting a genetic counselor. However, it is important to note that 95% of babies with spina bifida are born with no family history of the condition (4)>.
- Health conditions: Conditions such as diabetes and obesity during pregnancy might make one more prone to have a baby with spina bifida. Therefore, you must get to a healthy BMI range before getting pregnant and keep your blood sugar levels in check to avoid these conditions.
- Medications: Inform your doctor about any medicines that you consume. It includes prescription, OTC drugs, and herbal supplements. Avoid switching any medicines during pregnancy. Do not start or stop any medicines during pregnancy without doctor consultation. Some drugs, such as anti-seizure medicines, may increase the risk of having a baby with neural tube defects. If any healthcare provider is prescribing you medicines, make sure to inform your doctor about your pregnancy.
- Fever: A high body temperature may increase the risk of having a baby with spina bifida. If you develop a fever in the first six weeks of pregnancy, you must inform the doctor. Also, avoid using hot tubs and saunas if you are trying to get pregnant or are pregnant.
Symptoms Of Spina Bifida In Babies
According to the Stanford Children’s Hospital, the following are the symptoms of spina bifida in babies (5).
- Abnormal appearance of an area on the back, such as a small patch of hair, dimple, birthmarks, or a pouch-like bulge or a fluid-filled sac
- Loss of sensation below the area under the fluid-filled sac
- Inability to move legs or feet
- Constipation or urinary incontinence
Babies may also show symptoms such as:
- Increased fluid and pressure in the head (Hydrocephalus)
- Heart problems
- Bone problems
- Poor cognitive skills for their age
Symptoms of spina bifida occur differently in different babies. The symptoms may also be similar to other health conditions. Therefore, consult a doctor for a diagnosis.
Diagnosis Of Spina Bifida In Babies
Spina bifida can be diagnosed during pregnancy or after the baby is born. However, in some cases, it goes undiagnosed until late childhood or adulthood, or it may also go undiagnosed for the entire life.
The following are the diagnostic tests for spina bifida in babies during pregnancy (6).
- Blood tests: The triple screen or quad screen is a blood test done in the second trimester of pregnancy. It measures the amount of alpha-fetoprotein (AFP) passed into the mother’s body from the baby’s body. A high level of AFP may indicate spina bifida in babies. The AFP levels are elevated in about 75-80% of pregnant women who carry a baby with spina bifida.
- Ultrasound: Problems with spina bifida may be seen during ultrasound imaging scans. Your doctor may call you for ultrasound scans at different stages of pregnancy to confirm the presence of spina bifida.
- Amniocentesis: The doctor takes a small sample of amniotic fluid from the womb. The fluid is tested for AFP. High levels of AFP might indicate spina bifida in babies.
At times, spina bifida goes undiagnosed during pregnancy. However, it comes to the notice of doctors when they observe a patch of hair or dimple on the baby’s back after they are born. In such a scenario, they might use imaging scans such as X-ray, MRI, or CT scan to get a clear picture of the baby’s spine and bones of the spinal cord.
Treatment For Spina Bifida In Babies
Spina bifida is treated surgically either before or after the baby’s birth. The stage at which the condition is treated depends on various factors such as the gestational age, the position of the anomaly on the spine, and various other maternal health factors. The following are the notable attributes of prenatal and postnatal surgical treatment for spina bifida in babies (7).
1. Prenatal surgery
Prenatal surgery is performed for meningocele or myelomeningocele while the baby is still in the mother’s womb. It is a very delicate procedure that involves entering the uterus surgically and closing the opening in the spinal cord. Fetal surgeries show better results than postnatal surgeries.
Spinal cord damage is a progressive condition and treating it as early as possible yields better results. Therefore, prenatal treatment may be preferred in most cases.
2. Postnatal surgery
If the doctor decides to go for a postnatal surgery, they will monitor your pregnancy and plan for cesarean delivery at 37 weeks (2). Surgical repair of spina bifida is done 24 to 48 hours after birth and is done under general anesthesia. The surgeons will remove the meningocele or myelomeningocele if it is present and close the surrounding tissue and skin over the lesion to protect the spinal cord. The baby will be under the doctor’s observation in the NICU after the surgery.
Complications Of Spina Bifida In Babies
The following complications may occur due to spina bifida.
Muscle weakness or joint pain due to nerve damage to the lower body
- Paralysis of legs or feet
- Bowel problems, such as problems with bowel control
- Hydrocephalus, the accumulation of excess cerebrospinal fluid in the brain
- Chiari malformation type II, a condition where the lower part of the brain sits in the upper part of the neck
- Meningitis, a swelling-causing infection of the tissues that surround the brain and the spinal cord
- Tethered spinal cord, where the spinal cord is attached to the spinal canal, causing the cord to stretch as the baby grows
- Skin problems, such as callous formation, sores, or blisters, especially on the hips, ankles, or feet
- Latex allergy, including to latex toys and teethers
- Urinary tract infections (UTIs), often due to poor bladder and bowel control
Most complications can be managed with relevant lifestyle changes, such as avoiding latex toys and ensuring the right sleep posture for the baby to prevent skin sores. Exercises can help improve muscle strength and may reduce the risk of paralysis. UTIs can be managed with antibiotics, while complex complications, such as hydrocephalus and tethered spinal cord, require surgical correction.
Prognosis Of Babies With Spina Bifida
Spina bifida is a lifelong condition with no cure but can be managed with timely treatment. Many children with spina bifida live an active and productive life, with an insignificant difference in academic performance compared to children without spina bifida (4). Children with irreversible paralysis and severe movement problems may require wheelchairs and other aids for mobility.
About 85 percent of children need shunts to drain the spina bifida fluid, and about 45 percent of them develop some complications in the first year. Complications can be managed with timely intervention. Nearly 14 percent of children with spina bifida may not survive beyond five years (3).
Frequently Asked Questions
1. Can a baby with spina bifida walk?
If the spina bifida affects a part of the spine near the head, babies may have paralyzed legs. However, if it occurs near the hips, babies may be able to walk with or without any devices. Early treatment and physical therapy may help strengthen babies’ legs and increase movement and flexibility (8).
2. At what stage of pregnancy does spina bifida occur?
Spina bifida occurs in the first four weeks of pregnancy. Since many women have unplanned pregnancies and are unaware of conception during this time, it is recommended that they start taking 400 mcg of folic acid during their child-bearing age to prevent this condition (9).
3. Can a baby with spina bifida crawl?
Babies with spina bifida may start crawling. However, since the movement and sensation in their limbs are different, they may need more support and encouragement to do so (10).
Contact your child’s healthcare provider if you notice any new symptoms or symptoms that do not resolve or worsen. Follow-up of the child is essential. The common causes of deterioration are often curable if diagnosed and intervened in time. Seek your pediatrician’s guidance to help your child live their lives with self-esteem and maximum possible independence.
Key Pointers
- Spina bifida in babies occurs when the vertebral column is not formed properly, resulting in a gap.
- Inadequate maternal folic acid, genetic problems, and gestational diabetes are some factors that may increase the risk of spina bifida.
- Inability to move legs, abnormal bulge on the back, and bone problems are a few symptoms of this condition.
References
- Spina Bifida
https://www.marchofdimes.org/complications/spina-bifida.aspx - What is Spina Bifida?
https://www.cdc.gov/ncbddd/spinabifida/facts.html - Spina Bifida Causes Symptoms and Treatment
https://www.chop.edu/conditions-diseases/spina-bifida - Spina Bifida
American Association of Neurological Surgeons - Spina Bifida in Children
https://www.stanfordchildrens.org/en/topic/default?id=spina-bifida-90-P02415 - Spina Bifida
https://my.clevelandclinic.org/health/diseases/8719-spina-bifida - Fetal Surgery for Spina Bifida (Myelomeningocele)
https://www.chop.edu/treatments/fetal-surgery-spina-bifida - Living with Spina Bifida: Infants.
https://www.cdc.gov/ncbddd/spinabifida/infant.html#:~:text=Mobility%20and%20Physical%20Activity&text=Those%20with%20spina%20bifida%20lowerwith%20spina%20bifida%20is%20born - Folic acid now.
https://www.cdc.gov/Images_-_Video_and_Audio/Images/Folic_Acid/QandAfactfolic.pdf - Early mobility and the role of physiotherapy in spina bifida.
https://www.shinecharity.org.uk/what-to-expect/early-mobility-and-the-role-of-physiotherapy#:~:text=Spina%20bifida%20and%20early%20mobility%20%2D%20nine%20months%20to%20three%20years&text=They%20may%20start%20crawling%20andin%20order%20to%20do%20this.

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Dur Afshar Agha