Spinal Muscular Atrophy In Babies: Types, Symptoms & Treatment
Depending on the type of SMA in babies, the symptoms may vary from mild to severe.
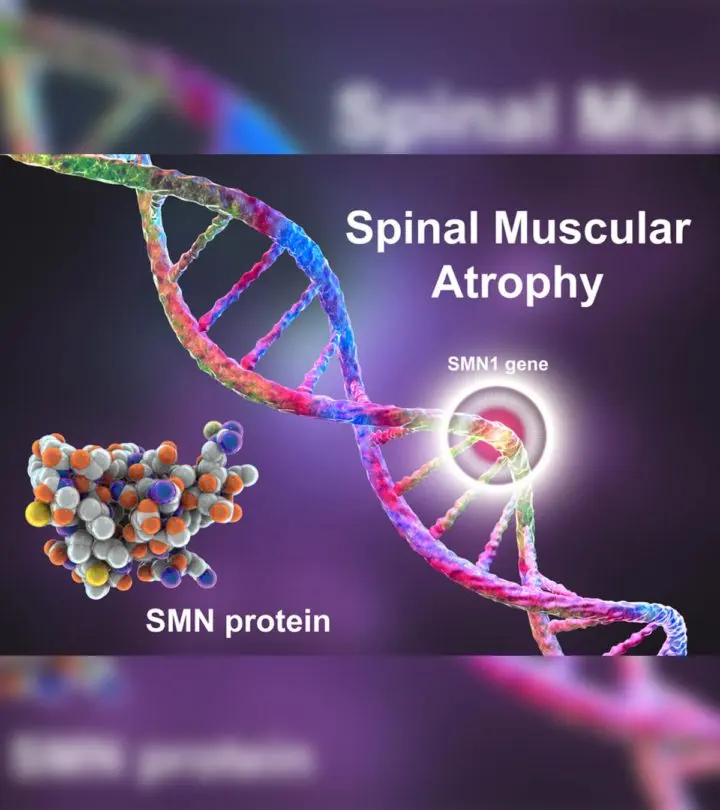
Image: Shutterstock
In This Article
Spinal muscular atrophy or SMA in babies is characterized by loss of motor neuron function. The condition is an uncommon genetic disorder where the motor neurons that control muscular function shrink and waste away (atrophy). The atrophy leads to improper signal reception (1) (2).
Usually, babies with SMA express the symptoms early in life. However, these symptoms may worsen and become noticeable with time (3). Learn more about the causes of SMA, its symptoms, and treatment in this post.
How Common Is SMA In Babies?
SMA affects one in 6,000 to 10,000 babies born in the United States. It is estimated that 10,000 to 25,000 children and adults with SMA live in the USA. The disorder is considered a rare disease(4)(1).
Types And Signs Of SMA
SMA is classified into different types based on the severity of the symptoms and the stage at which they are evident. Below are the signs and other salient attributes of different types of SMA (2)(5).
Type 0 (Severe)
- It is the most severe form of the disease and usually evident at birth.
- The affected infants may show less activity in-utero, causing them to be often born with joint deformities(contractures).
- They may have a very low muscle tone at birth.
- The baby may have extremely weak respiratory muscles.
- Some infants with SMA type 0also have congenital heart defects.
- The life expectancy of babies with type 0 is very poor, and most do not survive beyond a few months.
Type 1 (Acute)
- It is also known as Werdnig-Hoffman disease and is the most common form of SMA in babies.
- The symptoms are usually acute, severe, and evident at birth.
- Some affected babies may not show symptoms at birth but will develop them before six months.
- Most infants affected by SMA type 1 cannot sit unsupported and do not have head control.
- The baby may have difficulty with sucking and swallowing, causing feeding problems and poor growth.
- The baby may show tongue twitching.
- There may be issues with breathing due to weak respiratory muscles.
- The baby may have a bell-shaped chest, which hinders lung expansion, leading to respiratory problems
- The intelligence and cognitive functions are usually not affected.
- Many children with SMA type 1 do not survive past two years of age due to respiratory failure.
Type 2 (Intermediate)
- It is also called Dubowitz disease, and the signs are usually evident between the ages of six and 18 months.
- A baby with SMA type 2 can sit without support but may need assistance to get into the sitting position.
- This type mostly affects the leg muscles. Therefore, babies with SMA type 2 cannot stand or walk independently.
- The baby may exhibit involuntary tremors in their fingers.
- Some infants may display an abnormally curved spine (scoliosis).
- Respiratory muscle weakness may also be noticed.
- Life span depends on the condition’s severity. Many survive up to young adulthood(twenties or thirties) or beyond.
Type 3 (Mild)
- It is also called Kugelberg-Welander disease, and muscle weakness is seen in late toddlerhood, after 18 months of age.
- Those affected by SMA type 3 may walk and stand unsupported on an even surface for a short duration.
- The child may be unable to walk on uneven surfaces. Toddlers with SMA type 3 cannot walk up and down the stairs.
- The toddler may show partial abilities. For instance, they may be able to sit on a chair but cannot rise from it.
- The symptoms may worsen with time, causing the toddler to lose the ability to walk entirely. Most patients need wheelchair assistance eventually.
- Most toddlers with SMA type 3 have a normal life expectancy.
Note: SMA type 4 exists but occurs in adults, usually after the age of 35 years.
Causes Of SMA In Babies
SMA occurs due to mutations in the survival of motor neuron 1 (SMN1) and survival of motor neuron2 (SMN2) genes located on chromosome 5. The SMN1 and SMN2 genes provide the relevant instructions to the body’s cells to produce the survival motor neuron(SMN) protein. SMN protein is vital for maintaining motor neurons, which transmit nerve signals from the brain and spinal cord to the skeletal (voluntary) muscles(2).
People with SMA have a missing or mutated SMN1 or SMN2 gene. In most cases, they are missing a section of the SMN1 gene. Partial expression of the SMN genes leads to insufficient SMN protein, causing motor neurons to shrink and die. The brain and spinal cord cannot control skeletal muscles without motor neurons. The lack of nerve signals to the muscles causes them to experience atrophy, that is, they shrink and waste away. This condition is called SMA.
SMN1 gene is responsible for most of the SMN protein, with the SMN2 gene responsible for a small amount. Most individuals have two copies of the SMN1 gene and one to eight copies of the SMN2 gene. People with SMA and with a higher number of SMN2 genes may experience milder symptoms due to SMN2 genes compensating for the missing or mutated SMN1 gene. Generally, the milder the type of SMA, such as type 3, the higher the likelihood the person has more copies of SMN2 genes (1).
Diagnosis Of SMA
Pregnant women with a family history of SMA may go for prenatal tests, such as amniocentesis and chorionic villus sampling, to check if the fetus is at risk of developing SMA. These tests may be suggested if the healthcare provider notices poor fetal activity during an ultrasound scan.
If symptoms are noted after childbirth, the doctor will first perform simple tests and examinations to distinguish between spinal muscular atrophy(SMA) and other similar conditions, such as muscular dystrophy. To confirm the diagnosis, the doctor may order the following tests(6).
- Blood tests: The elevated levels of creatine kinase (CK) enzyme in the blood indicate degenerating skeletal muscles. It is not a specific test for SMA but lets the doctor confirm that the muscles are wasting away.
- Nerve conduction test: An electromyogram may be performed to measure the speed at which electrical signals travel along the nerves. An electromyogram may also be performed to measure the electrical activity within the muscles.
- Genetic testing: If prior tests suggest SMA, the doctor will order genetic testing. A blood sample is withdrawn and assessed for anomalies in the SMN1 and SMN2 genes.
Management Of SMA In Babies
There is no cure for SMA. Certain treatment strategies work at making the symptoms milder and manageable, improving the baby’s quality of life. The doctor may suggest any of the following methods to manage SMA in babies, depending on their symptoms and type of SMA (7).
1. Gene replacement therapy
The baby’s healthcare provider may suggest a gene replacement or modification therapy. A common gene replacement therapy medication used in babies younger than two years is onasemnogene abeparovec known by its brand name Zolgensma. The injectable medication is made of a benign virus, which delivers the healthy SMN1 gene to the targeted motor neuron cells, improving their function. It eventually leads to better muscle control and health.
Risdiplam, known by its brand name Evrysdi is an oral medication that modifies the SMN2 gene to make it more efficient at producing SMN protein. An increased quantity of SMN protein improves motor neuron functions and muscle health eventually. The medicine is recommended for babies two months and older.
2. Physical therapy
The baby may be recommended various physical therapies that parents may help perform. Physical therapy could consist of different exercises suggested based on the baby’s age and type of SMA. Some exercises may require parents to visit a professional who may perform the exercises with specialized equipment.
Regular physical therapy sessions may help improve joint mobility, slow down muscle atrophy, and improve posture.
3. Assistive techniques
Braces and wheelchairs could be provided to the baby as they grow older to improve their quality of life. Appropriate nutrition through a customized diet plan could also improve health, making the effects of SMA manageable.
Complications Of SMA
People with SMA experience progressive muscle weakness and loss of muscle control. It may lead to the following complications in the long run (1).
- Respiratory infections
- Weak lungs and breathing problems
- Bone fractures
- Hip dislocation
- Scoliosis
- Malnutrition and dehydration due to problems with swallowing
How To Prevent SMA In Babies?
If you or your partner has a family history of SMA, you may visit a genetic counselor. The counselor may recommend preimplantation genetic diagnosis (PGD), depending on your risk of having a baby with SMA. PGD involves profiling embryos for healthy SMN genes. PGD works in conjunction with in vitro fertilization (1).
Once an embryo with healthy genes is found, it is implanted into the uterus for pregnancy. Since the embryo has healthy genes, it negates the chances of having a baby with SMA even if you or your partner has a family history of it.
Frequently Asked Questions
1. Are babies tested for SMA at birth?
Early diagnosis and start of treatment may improve prognosis in children with SMA. Hence, many hospitals in the USA have started testing babies for SMA at birth to improve treatment outcomes and prevent mortality (8).
2. Can children with SMA talk?
Children with SMA can talk, but SMA type 1 can affect a child’s ability to pronounce words or speak a language clearly (9).
The primary cause of SMA in babies is the missing chromosome in one of the motor neurons that affect the transmission of signals from the brain to the spinal cord. Before birth, SMN can be diagnosed with the help of prenatal tests, and if the symptoms appear after birth, they can be diagnosed by blood tests or genetic testing. However, timely intervention and proper medical care comprising gene replacement therapy or physical therapy based on the type of SMA can help prevent and manage its symptoms.
Key Pointers
- Signs of spinal muscular atrophy in babies include joint deformities, inability to sit, and difficulty in sucking or swallowing.
- It can be managed with the help of gene replacement therapy, physical therapy, and other assistive techniques.
- If your family has a history of this issue, you must visit a genetic counselor to avoid complications.
References
2. Spinal muscular atrophy; U.S. National Library of Medicine
3. About SMA Frequently Asked Questions; Spinal Muscular Atrophy Foundation
4. About SMA Overview; Spinal Muscular Atrophy Foundation
5. Spinal Muscular Atrophy; National Organization for Rare Disorders
6. Spinal Muscular Atrophy (SMA); Muscular Dystrophy Association
7. Spinal Muscular Atrophy Fact Sheet; National Institute of Neurological Disorders and Stroke
8. Newborn Screening for Spinal Muscular Atrophy; U.S. Health Resources & Services Administration
9. Grazia Zappa et al.; Intellectual abilities, language comprehension, speech, and motor function in children with spinal muscular atrophy type 1; Journal of Neurodevelopmental Disorders

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Elham Raker