Strabismus In Children: Guide To Causes, Risks & Treatment
Eyeglasses, vision therapy, or surgery may help with eye alignment problems in kids.

Image: Shutterstock
Strabismus in children is a common ocular condition that affects around 2–4% of the population. It occurs when the eyes are misaligned and point in different directions while focusing on an item; hence, it is also known as crossed or squint eye.
The six muscles that regulate eye movement normally function together to point both eyes in the same direction. However, people with strabismus have trouble controlling their eye movement and cannot maintain the alignment of their eyes (eye position) (1).
In some children, strabismus is intermittent, while in others, it is permanent. If you believe your child has strabismus or other vision difficulties, seek medical help.
This post informs about the causes, risk factors, types, signs, symptoms, diagnosis, and treatment options for children with strabismus.
Causes Of Squint In Children
Some children are born with a squint or have a positive family history, while others may develop it later in life while the eye attempts to overcome vision problems. Squint commonly develops in children between the ages of 18 months and four years due to various reasons (2).
Some common causes of squint may include (2)
- Short-sightedness (myopia) or difficulty seeing distant objects clearly.
- Long-sightedness (hypermetropia) or difficulty seeing nearby objects clearly.
- Astigmatism, an abnormally curved eye that causes blurred vision.
Some rare causes of strabismus in children may include (2)(3)
- Some infections, such as measles
- Some genetic conditions, such as Down’s syndrome
- Cerebral palsy and other brain and nerve abnormalities
- Symptom of retinoblastoma, a childhood eye cancer
- Eye muscle problems such as Brown’s syndrome, where an eye does not move upwards, and Duan retraction syndrome, where both eyes do not turn to the sides well.
You may consult a pediatric ophthalmologist to know the exact cause of strabismus in your child. Early interventions can prevent vision impairment and other complications in many children.
Risk Factors For Cross Eyes
The following factors may increase the risk for strabismus in children(4).
- Prematurity
- Retinopathy of prematurity (ROP)
- Genetic factors and family history of strabismus
- Anisometropia (unequal refractive power in the two eyes)
- Hyperopia (farsightedness)
- Maternal smoking during pregnancy
- Low birth weight
- Cerebral palsy
- Stroke
Although many risk factors are not modifiable, high-risk factors such as maternal smoking during pregnancy can be modified.
Types Of Strabismus
Strabismus can be classified into three categories depending on the direction of the eye misalignment (5).
- Infantile esotropia: This refers to an inward (towards the nose) turning of one or both eyes seen in babies and young children
- Exotropia: It is the outward (away from nose) turning of eyes while looking at far objects. This may also occur when the child is tired or sick.
- Accommodative esotropia: This is when one eye turns inward towards the nose while focusing on distant or close objects. This is the most common type of strabismus seen in children older than two years.
Signs Of Crossed Eyes In Children
The signs and symptoms of strabismus can come and go and often worsens when a child is ill or tired. Visit a pediatric ophthalmologist (eye specialist) if your child has any signs of strabismus.
The common signs of strabismus in children may include (6)
- Eyes that do not point in one direction at the same time. Mild misaligned eyes may go unnoticed.
- Closing or squinting one eye often in bright sunlight.
- Eyes that do not move together.
- Bumping into things due to limited depth perception.
- Turning or tilting the head to look at an object that is visible with moving eyes.
Older children with strabismus may suffer from the following symptoms.
- Tired eyes
- Blurred vision
- Double vision (diplopia)
- Photosensitivity (sensitivity to light)
In a few cases, a wide nose bridge or a fold of skin at the inner eyelid can make the eyes look crossed. You may consider this factor while looking for signs of strabismus in children.
Complications Of Crossed Eyes
The possible complications of strabismus may include (1)
- Lazy eye (amblyopia). It refers to the lack of vision development in one or both eyes. If left untreated, lazy eyes may result in vision loss.
- Double vision (diplopia). This is commonly seen in older children with acquired strabismus (strabismus occurred in later life).
- Poor self-esteem. The appearance of the eyes may cause socializing problems and poor self-esteem in older
Early diagnosis and treatment of strabismus can prevent vision problems and blindness in children.
Diagnosis Of Strabismus
Diagnosis of strabismus can be made via eye examinations. Periodical eye examinations are recommended during infancy and between the ages of three and five years to measure vision and diagnose strabismus and other ophthalmic conditions.
In young children, doctors may shine the light into the eye to look for light reflexes and observe their eye movements. Older children are examined by asking them to read letters by covering one eye and with lenses.
Imaging tests such as magnetic resonance imaging (MRI) and computed tomography (CT) are often ordered to determine any underlying causes such as neurological conditions. Genetic testing may also be done by analyzing blood to identify genetic disorders that cause vision problems (5)(7)(8).
Treatment For Strabismus In Children
The following treatment options for strabismus may help improve eye alignment and coordination. Doctors may recommend orthoptics treatments (non-surgical treatments) for most children with mild misalignments. These may include the following (7)(8).
- Eyeglasses and contact lenses may be the only treatment required in some
- Prism lenses are thicker on one side than the other. This may alter the light entering the eyes and help reduce eye turning to view objects.
- Vision therapy includes structured visual activities that help the eyes and brain to work together. This is usually done under the supervision of an optometrist.
- Eye muscle surgery helps change the position or length of muscles around the eyes to give them a straight appearance. After an eye muscle surgery, some children may require vision therapy to improve eye-brain connection and prevent the recurrence of eye misalignment.
- A temporary eye patch is often placed over the stronger eye if one eye has amblyopia (lazy eye).
- Atropine eye drops are also prescribed for chemical ocular (eye) patching in some children with strabismus. This causes temporary blurred vision in the unaffected eyes and enhances the alignment of deviated eyes.
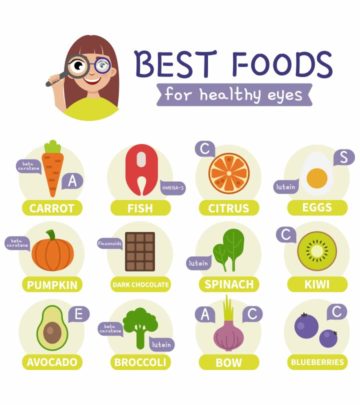
- Other medications such as botox (botulinum toxin type A) injections are also given to weaken the overactive eye muscles. This is often done with or instead of other treatments. Uncorrected strabismus can have far-reaching effects, including loss of vision and stereoacuity, and adverse effects on psychosocial development and gainful employment. Esotropia, in general, is most urgent in terms of requiring immediate attention to manage any vision loss or adverse effects on stereoacuity. Interventions at an early age are shown to improve vision and prevent complications associated with strabismus in children
Frequently Asked Questions
1. Can a child outgrow strabismus?
Pseudostrabismus or false strabismus is a condition where a baby’s eyes may seem misaligned when they are actually not. This condition resolves as the child grows. However, children do not usually outgrow true strabismus, and the condition may deteriorate without treatment (8).
2. Is strabismus a birth defect?
It is not always a birth defect. Children may be born with strabismus or acquire the condition later in life (1).
3. Is strabismus the same as lazy eye?
Lazy eye or amblyopia is not the same as strabismus. Lazy eye occurs when vision is impaired due to poor functional coordination between the brain and eyes. Whereas, strabismus is eyes’ misalignment, which is one of the causal factors for lazy eyes (9).
Premature birth, low birth weight, hyperopia, anisometropia, and various ocular and genetic abnormalities are linked to an increased risk of strabismus in children. Don’t assume the child will outgrow it because, while strabismus can be intermittent in some children, it can also be permanent in others. If a lazy eye develops and is not treated on time, a kid with strabismus may also experience permanent vision loss. So, make sure to get your child’s eyesight checked before six months and again between three and five years. Although strabismus is unavoidable, early detection and treatment may assist in avoiding such complications.
Key Pointers
- Strabismus or squint in children may occur from birth or develop over time due to vision problems.
- The causes of squint include short- or long-sightedness and developmental delays.
- Some signs of crossed eyes are the inability to move the eyes together and squinting an eye in sunlight.
- The treatment options include eyeglasses, prism lenses, and vision therapy.
References
2. Childhood squint (strabismus); Royal National Institute of Blind People (RNIB)
3. Squint; National Health Service
4. Gail D. E. Maconachie
5. Strabismus In Children; American Academy of Ophthalmology
6. Strabismus (Crossed Eyes) Symptoms; Stanford Health Care
7. Strabismus (Crossed Eyes): Cleveland Clinic
8. Strabismus (crossed eyes); American Optometric Association
9. Lazy Eye (Amblyopia); Johns Hopkins Medicine
Read full bio of Dr. Dur Afshar Agha