Tetralogy Of Fallot In Babies: What It Is, Symptoms & Treatment
Tetralogy of Fallot symptoms in babies can be managed with prompt diagnosis and treatment.
In This Article
The prevalence of Tetralogy of Fallot in babies is uncommon, occurring in around one in every 3,000 live births. It is a heart condition consisting of four congenital heart defects that ultimately disrupt the normal blood flow from the heart to the lungs and the body. Heart defects in the Tetralogy of Fallot (TOF) can impede blood circulation from the right ventricle and shunt deoxygenated blood from the right to the left ventricle. As a result, low oxygen levels in the body and cyanosis in babies are possible outcomes.
If left untreated, TOF can cause life-threatening complications; however, it has a better prognosis after surgical correction and ongoing follow-ups.
Read on to know the causes, symptoms, complications, diagnosis, and treatment for TOF in babies.
Heart Defects In Tetralogy Of Fallot
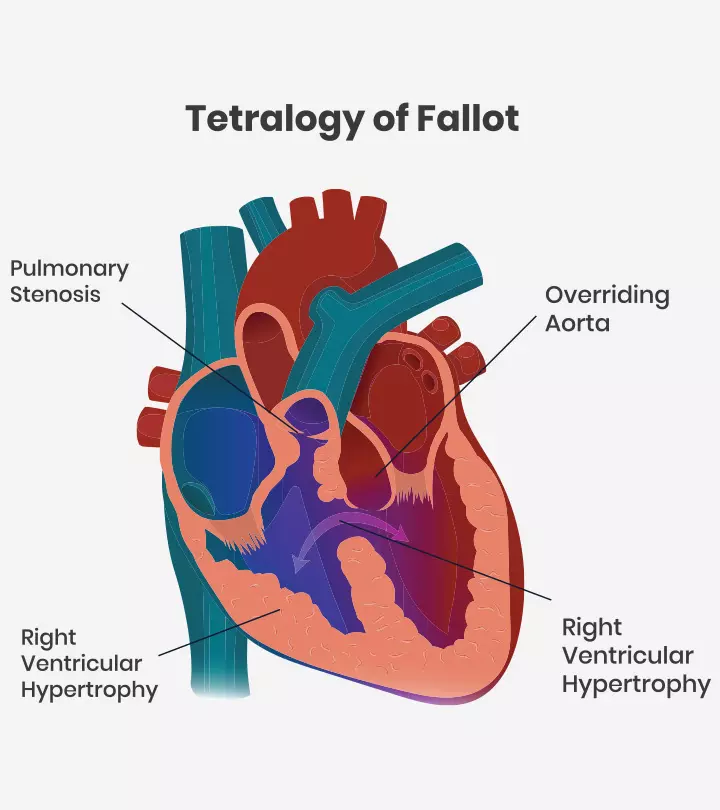
Tetralogy of Fallot involves four major congenital heart defects (1).
- Ventricular septal defect (VSD) is a hole between the heart’s left and right ventricles (lower chambers).
- Pulmonary stenosis is the narrowing of the pulmonary valve.
- Overriding aorta is a condition in which the aorta that connects to the left ventricle of the heart is placed farther to the right. In TOF, the aorta is positioned between the left and right ventricles over the ventricular septal defect.
- Right ventricular hypertrophy is the thickening of the myocardium (muscular wall) of the right ventricle.
In addition to these defects, abnormalities in coronary artery branching and atrial septal defects (ASD) are seen in a very small percentage of babies with TOF. Some babies may have pulmonary atresia, complete obstruction of the pulmonary valve, or this valve may not form at all. This may prevent blood flow from the heart to the lungs. Some babies may also have other non-cardiac birth defects.
What Happens In TOF?
Blood flow to the lungs can be limited in TOF due to pulmonary stenosis and related right ventricular outflow tract obstruction (RVOTO). Defects of the pulmonary valve and pulmonary artery in the supravalvar regions can cause RVOTO. In severe cases, blood flow to the lungs can be completely blocked (2).
In TOF, when there is an obstruction of blood flow to the lungs from the right ventricle, the poorly oxygenated blood begins to shunt from the right ventricle to the left ventricle through the ventricular septal defect. Therefore, poorly oxygenated blood is pumped from the left ventricle to the systemic circulation. In addition to this, overriding of the aorta also gets poorly oxygenated blood from VSD.
Shunting the oxygen-poor blood from right to left can cause low oxygen levels in the body, resulting in cyanosis. The severity of cyanosis may vary depending on the degree of pulmonary valve stenosis and RVOTO. Obstructed outflow from the right ventricle increases right ventricular pressure, and pumping against high pressure can lead to hypertrophy (thickening) of the right ventricle walls.
Signs And Symptoms Of Tetralogy Of Fallot
The following signs and symptoms of TOF are seen in babies (2).
- Loud and harsh murmur or cyanosis (bluish skin) can be initial symptoms of Tetralogy of Fallot in most babies. This is often diagnosed in the first few weeks of life.
- Low oxygen levels and decreased pulmonary blood flow can cause rapid breathing in babies.
- Most babies with TOF have failure to thrive, are tired while feeding, and have poor weight gain.
- Tetralogy spell is another common symptom of TOF in babies. This is the sudden marked drop in arterial oxygen saturation. Babies can be irritable in response to tetralogy spells initially, and they become sleepy or unresponsive if it persists.
Babies with patent ductus arteriosus (opening between two blood vessels) may not develop severe cyanosis (bluish skin) early since these vessels provide additional blood flow to the lungs. However, cyanosis may appear as soon as the ductus arteriosus closes, often occurring on the first day of life(2). Seek immediate medical care if your baby has tetralogy spells. Comforting the baby and flexing knees upward and forward may help in some cases.
Risk Factors And Causes For TOF
The exact cause of TOF is not known. It could be multifactorial, which means it could be a combination of genetic and environmental factors. The following factors may increase the risk of TOF in babies (3).
- Poor nutrition during pregnancy
- Maternal alcohol use
- Maternal viral illnesses
- Maternal diabetes
- Advanced maternal age (over 40 years)
Nearly 25% of babies with TOF also have other congenital birth defects not related to the heart. Babies with chromosomal abnormalities, such as Down syndrome, may often have a high risk of TOF and other congenital heart defects (3).
Complications Of TOF
Tetralogy of Fallot can interrupt normal growth in babies. If left untreated, the following complications may occur in some babies (4).
- Arrhythmias (abnormal heart rhythms)
- Right heart failure or heart failure
- Endocarditis
- Blood clots leading to stroke
- Sudden death
Seek immediate medical care if your baby has any symptoms of TOF, such as cyanosis, breathing difficulties, or trouble while eating or being active.
Diagnosis Of Tetralogy Of Fallot
A detailed history of symptoms and physical examination, including hearing murmur with a stethoscope, can be helpful in the diagnosis of TOF in babies. Pediatric cardiologists may order the following tests to confirm the TOF diagnosis (5) (6).
- Echocardiography is the ultrasound imaging of the heart to assess its structure and function. It could help visualize and locate the heart and valve defects, helping understand their severity.
- Electrocardiogram records the electrical activity using electrodes placed on the chest. Irregular heart rhythm is obtained if the baby has right ventricular hypertrophy (enlargement of the right ventricle).
- Chest X-ray also helps to visualize the structure of the heart and lungs. Enlarged right ventricle can give a boot shape to the heart on X-rays.
- Cardiac MRI or CT scans give more accurate images of the heart with size and function. This may often be done before planning cardiac surgeries.
- Cardiac catheterization is done to directly measure the pressure in the heart and to look for the structure. This can also be done for therapeutic purposes.
- Electrophysiologic study (EPS) is an invasive test to evaluate the heart’s conduction (electrical) system. Abnormal rhythms are identified in these tests. Pediatric electrophysiologists can map the location of problems in the heart, and it is often done at the same time as cardiac catheterization. However, EPS may cause complications in babies.
- Pulse oximetry measures the oxygen levels in the blood using sensors placed on the fingertips.
These diagnostic tests are needed for differential diagnosis of TOF since congenital heart disorders, such as atrioventricular septal defect (AVSD), atrial septal defect (ASD), and ventricular septal defect (VSD), can also have similar symptoms. In addition, rare conditions, such as congenital mitral valve stenosis, cor triatriatum (extra chamber above left atrium), and cor triloculare biatriatum (absence of one ventricle), are also excluded while diagnosing TOF in babies (3).
Treatment For TOF In Babies
Surgical repair is the only treatment for TOF in babies. Temporary procedures with shunt intracardiac repair are surgical options to repair TOF. Most babies and older children undergo intracardiac repair of the defects. Surgical procedures to repair TOF may include the following (7).
1. Intracardiac repair
Open heart surgery involving several repairs is required for TOF correction. During this procedure, the ventricular septal defect is closed with patches. Narrowed pulmonary arteries are widened, and pulmonary valves are replaced to increase the blood flow from the heart to the lungs.
Right ventricle thickness may go back to normal size after this procedure since the right ventricle does not have to work as hard to pump blood as before. The symptoms also improve after the repair procedure since the oxygen levels increase in the blood.
3. Temporary surgery
Doctors may opt for temporary (palliative) procedures to maintain blood flow if there are any contraindications to repair the baby’s health status. This is often done in premature babies and babies with hypoplastic (underdeveloped) pulmonary arteries. Shunt (bypass) is created between two large arteries branching from the aorta and pulmonary artery. This shunt is removed when the baby undergoes intracardiac repair in the future.
Most babies have a good prognosis after surgical repair of TOF. However, long-term complications, such as valve problems, arrhythmias, aortic root dilation, or coronary artery disease, may occur in some babies who undergo intracardiac repair for TOF.
Follow-Up And Care After TOF Repair
Babies require regular follow-ups and evaluation of new complications and cardiac functions even after TOF repair procedures. Pediatric cardiologists in childhood and adult congenital cardiologists in adulthood are specialists involved in the ongoing care of TOF. The ongoing care aims to identify complications and intervene earlier. It may include the following practices (7).
- Medical therapy, ablation, or placement of ICD (implantable cardioverter-defibrillator) or pacemaker is indicated for arrhythmias, depending on the severity and type.
- Doctors may recommend a preventive antibiotic course before surgical or dental procedures in children who underwent TOF repair. It is usually because prosthetic material, such as a ventricular patch or artificial valves, may increase the risk of endocarditis.
- Medications to prevent blood clots are also often prescribed, especially if atrial septal defects and arrhythmia are present.
- Strenuous activity restriction can also be recommended in some cases. You may ask the cardiologist to know about safe and effective exercises for your child to stay healthy.
- Good oral hygiene and regular dental checkups are also included in ongoing care for TOF.
Life Expectancy In Tetralogy Of Fallot
Life expectancy can be lower if the TOF is left untreated. However, the survival rate may vary depending on the severity of defects. More than 75% mortality within ten years is observed in untreated cases. However, those who underwent TOF corrective surgeries were shown to have more than 70% survival at 35 years (8).
Frequently Asked Questions
1. Can TOF be cured?
Babies diagnosed with TOF need corrective heart surgery. Depending on the severity of the condition, some babies may need more than one surgery. Most babies who receive timely treatment do well. However, they require regular follow-ups with a heart specialist to monitor their progress and check for other health conditions that might develop when the baby grows older (9).
2. What is the optimal age for correcting TOF?
Tetralogy of Fallot is a congenital heart defect, and symptoms can be present in the first week. Infants with cyanosis should be evaluated for underlying heart problems. Although tetralogy of Fallot is not preventable, timely management can prevent complications and improve the quality of life in babies. Ongoing care after cardiac repair plays a crucial role in the life expectancy of babies with TOF.
Key Pointers
- Tetralogy of Fallot (TOF) is a rare heart condition that involves four types of heart defects.
- The condition obstructs blood flow from the heart to the lungs and presents bluish skin, unresponsiveness, and decreased weight gain.
- TOF in babies may result from malnutrition in pregnancy, mother’s alcohol intake, or mother’s illness.
- The doctor may carry out a physical test of the baby and imaging modalities of the heart.
- Babies with TOC are treated by surgical methods and require good follow-up care.
References
- Tetralogy of Fallot.
https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects/tetralogy-of-fallot - Tetralogy of Fallot.
https://www.cincinnatichildrens.org/health/t/tof - Tetralogy of Fallot.
https://rarediseases.org/rare-diseases/tetralogy-of-fallot/ - Tetralogy of Fallot (TOF).
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=p01822 - Tetralogy of Fallot.
https://www.nationwidechildrens.org/conditions/tetralogy-of-fallot - Tetralogy of Fallot.
https://radiopaedia.org/articles/tetralogy-of-fallot - Tetralogy of Fallot.
https://www.stclair.org/services/mayo-clinic-health-information/diseases-and-conditions/CON-20316969/ - Tetralogy of Fallot without Corrective Surgery in a 33 year-old ICU Patient.
https://pediatrics.aappublications.org/content/140/1_MeetingAbstract/47 - Facts about Tetralogy of Fallot.
https://www.cdc.gov/ncbddd/heartdefects/tetralogyoffallot.html - Pediatric Tetralogy of Fallot (TOF).
https://childrensnational.org/visit/conditions-and-treatments/heart/tetralogy-of-fallot-tof

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.
Read full bio of Dr. Dur Afshar Agha