7 Causes Of Ulcerative Colitis In Children, Signs And Treatment
Some of the causes of ulcerative colitis in children may be controllable.
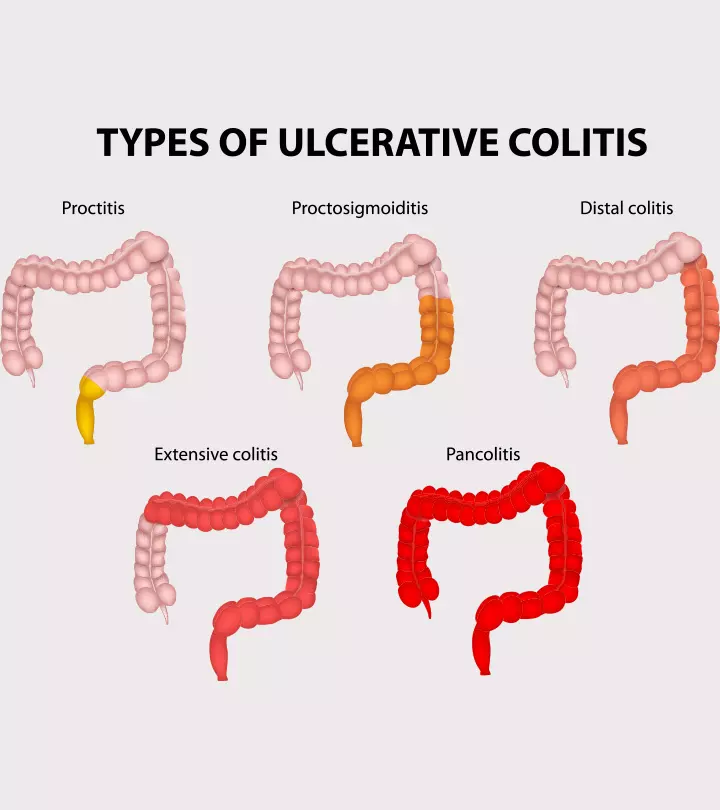
Image: Shutterstock
In This Article
Ulcerative colitis in children is a type of inflammatory bowel disease (IBD), which causes chronic inflammation of the inner layers of the large intestine (colon). The inflammation may start from the rectum or lower parts of the colon, spreading across the inner layers of the colon gradually. Ulcerative colitis is considered one of the IBDs along with Crohn’s disease (1).
Poorly managed ulcerative colitis in children may affect the nutrients their intestines absorb, leading to other complications, such as poor physical and cognitive development. The symptoms may also become more aggressive than in adults (2).
Read this post to learn the various causes, symptoms, and treatment options for ulcerative colitis in children.
Incidence Of Ulcerative Colitis In Children
According to Dr. Dinesh Pashankar, director of Yale Medicine’s Pediatric IBD Program, “An estimated 80,000 children in the United States suffer from IBD, about half of whom have ulcerative colitis (3).”
According to a study, out of around one million people in the US with IBD, approximately 20–25% of those diagnosed with ulcerative colitis are under 20 years. Furthermore, the incidence of ulcerative colitis in children increases every year (2) (4).
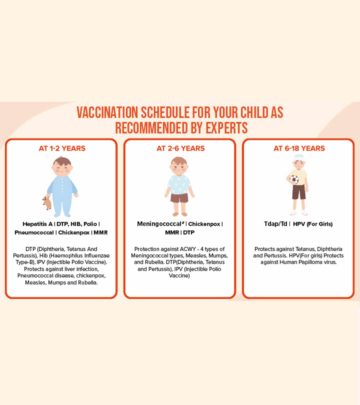
Types Of Ulcerative Colitis
There are mainly three types of ulcerative colitis based on the site of inflammation (2) (3):
- Ulcerative proctitis is a milder form of the disease that mostly affects adults and causes inflammation limited to the rectum.
- Pancolitis is the most common type of pediatric ulcerative colitis and causes the entire colon to be inflamed.
- Distalcolitis results in inflammation in the left side of the colon.
Causes And Risk Factors Of Ulcerative Colitis In Children
The exact cause of ulcerative colitis in children is unknown. The causes of pediatric ulcerative colitis may be multifactorial, involving genetic, immunologic, and environmental factors (5).
The following factors may increase the risk of contracting ulcerative colitis in some children (1) (3):
- Family history: Either parent or any siblings (first-degree relatives) have ulcerative colitis
- Age: While the possibility of contracting ulcerative colitis is lower in children than in adults, children above 15 years are at an increased risk of developing this condition, irrespective of gender.
- Ethnicity: Whites and individuals of Eastern European (Ashkenazi) Jewish descent have the highest risk.
- Environment: More common in urbanized, industrialized areas than in developing countries, indicating that a high-fat, refined-food diet could be a factor. It’s also more prevalent in colder climates.
- Immunologic: Often, children with ulcerative colitis face disturbances in their immune system function. Hence, it may be an autoimmune disease (where the immune system attacks its own cells). However, it is unknown whether these immunologic changes are the result or the cause of ulcerative colitis in children.
- Altered microbial gut flora: Viral or bacterial invasion may trigger ulcerative colitis in children, causing intestinal wall inflammation.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Although NSAIDs, such as ibuprofen, diclofenac, and naproxen, do not cause ulcerative colitis, they may increase the risk of intestinal inflammation in some children.
Symptoms Of Ulcerative Colitis In Children
Ulcerative colitis manifests itself in various ways; however, the most prevalent symptoms of ulcerative colitis in children include (1) (3)
- Stomach pain
- Bloody diarrhea (Hematochezia)
- Bowel urgency
- Fatigue
- Cramping
- Weight loss
- Appetite loss
- Rectal bleeding
- Body fluid and nutrient loss
- Anemia from severe bleeding
Further, constipation can be an early indication of ulcerative colitis in children (2). In addition to gastrointestinal (GI) symptoms, the affected child may present atypical symptoms, including (1) (3)
- Swelling (edema) and joint pain
- Mouth and skin sores (lesions)
- Osteoporosis
- Red, painful, and itchy eyes
- Kidney stones
- Liver problems
Ulcerative colitis is a chronic condition; hence, an affected child may experience periods of no symptoms (remission) after periods of active symptoms (flare). This remission can extend for months or years, but the symptoms will eventually return. Mild symptoms may appear first, while severe symptoms may appear later in some children (1) (3).
When To See A Doctor
You should contact your child’s health care provider in the following scenarios (1):
- You have noticed symptoms of ulcerative colitis in your child
- Your child develops new symptoms during treatment
- Your child has a flare-up
- You are concerned about your child’s growth
Diagnosis Of Ulcerative Colitis
Many symptoms of pediatric ulcerative colitis are common in other conditions. Hence, when your child is suspected of having the condition, your health care provider may first rule out other possible causes.
The diagnostic workup may include a standard physical examination and the child’s family and clinical history (3). In addition, the following laboratory tests may help diagnose ulcerative colitis in children (1) (6):
- Blood tests to check for anemia or a high white blood cell count (a sign of inflammation)
- Stool samples for signs of hematochezia (bloody stools) or bacterial or parasitic infections
- Imaging studies, including magnetic resonance enterography (MRE) and video capsule endoscopy, to provide a detailed picture of the small intestine without unnecessary exposure to radiation (7).
- Upper endoscopy (esophagogastroduodenoscopy or EGD), where a thin, flexible, lighted tube (endoscope) is directed through the mouth and throat into the esophagus, stomach, and duodenum for examination and sample collection.
- Colonoscopy, where a colonoscope is inserted into the rectum and moved up to the colon to detect abnormal growths, inflamed tissues, ulcers, or bleeding and for sample collection.
- Biopsy entails the surgical removal of a tissue sample from the intestinal lining for microscopic examination.
- Barium enema (lower GI series) involves inserting a tube containing a thick, chalky fluid called barium into the child’s rectum to check the large intestine, including the colon and rectum.
Treatment For Ulcerative Colitis In Children
The treatment for ulcerative colitis in children may vary as per the child’s symptoms, age, and general health and the severity of the condition. It may include (6):
- Diet: Diet changes are unlikely to benefit this condition. However, avoiding certain foods that irritate your child’s stomach may help reduce their symptoms, especially during a flare.
- Medicine: It is the primary treatment method, often used to reduce colon inflammation. Aminosalicylates, steroids and immunosuppressants, antibiotics, immunomodulatory therapy, and biologic medicines are used (3).
- Hospitalization: The symptoms of ulcerative colitis in children are typically moderate to severe, necessitating hospitalization to ensure proper nutrition, stop diarrhea, and prevent blood, fluid, and mineral loss. Your child may require a specific diet, intravenous feeding, or medicines.
- Surgery: Surgery may be required in case of excessive bleeding, colon tear (perforation), cancer risk, or severe illness. Surgery may also be suggested if your child’s symptoms don’t respond to other therapies or if they develop complications. Unlike Crohn’s disease, where surgery is a temporary solution, it can provide long-term remission in ulcerative colitis (5).
Your child may have one of the following surgeries:
- Proctocolectomy is the most common surgical method in children, where the entire colon and rectum are removed. It is followed by an ileostomy, where the surgeon creates a small incision in the abdominal wall, and the tip of the lower small intestine (ileum) is brought to the skin’s surface to allow waste drainage.
- Ileoanal anastomosis comprises the removal of the afflicted portion of the colon. The ileum is attached to the inside of the rectum, forming a pouch to hold the waste. This allows your child to pass stool normally through the anus. However, your child’s bowel movements may be more frequent and watery than usual.
Complications Of Ulcerative Colitis In Children
Death due to ulcerative colitis is rare. Other complications of ulcerative colitis in children may include (1) (8)
- Increased risk of developing colon cancer if the inflammation spreads beyond the rectum and lower colon
- Increased risk of colon tear (perforation)
- Periods of heavy bleeding
- Weight loss due to low food intake, increased gastrointestinal losses, and higher energy expenditure from chronic inflammation
- Increased risk of developing extra-intestinal manifestations such as erythema nodosum and pyoderma gangrenosum
- Liver problems such as drug-induced hepatitis, autoimmune hepatitis, or sclerosing cholangitis due to long-term pharmacotherapy for ulcerative colitis
- Musculoskeletal symptoms, such as mild arthralgia or severe spondyloarthropathies, especially in children positive for human leukocyte antigen B27 (HLA-B27)
In addition, the child may experience various physical, emotional, and social issues because of the recurrence of the condition. It may also affect the parents and other family members (7).
Tips For Parents To Manage Ulcerative Colitis In Children
Because ulcerative colitis is a chronic illness, your child may require long-term care. Here are some suggestions to help manage your child’s condition (1):
- Identify the foods that trigger your child’s condition.
- Ensure your child receives adequate nutrition for proper growth and development.
- Create a care plan with your child’s healthcare provider.
- Look for new symptoms and flare-ups and contact your child’s doctor.
- Understand why your child needs a particular test, medicine, or treatment and whether they have any negative effects.
- Research about the available resources and support groups for you and your child.
Frequently Asked Questions
1. Is colitis a serious disease?
Colitis is not fatal and can be acute or chronic; however, depending on the type of colitis, it can be severe and chronic, resulting in complications such as toxic megacolon and encephalopathy (9).
2. What’s the difference between colitis and ulcerative colitis?
Colitis is an acute or chronic inflammation of the mucosal lining of the colon and can be caused due to various factors, including infections, certain drugs, or secondary to immunodeficiency diseases. However, ulcerative colitis is a more severe chronic condition and is a type of inflammatory bowel disease (IBD) (9) (10).
3. At what age is colitis diagnosed?
Ulcerative colitis is the chronic inflammation of the large intestine and rectum. Children aged 15 years and older are more likely to develop this condition, though family history and genetic predisposition may also increase the risk of developing it. The symptoms of ulcerative colitis in children include bloody diarrhea, abdominal pain, and weight loss. The treatment mainly includes proper nutrition, medicines, and sometimes, surgery.
Key Pointers
- Ulcerative colitis in children is an inflammatory condition with three different types.
- The precise cause for ulcerative colitis is unknown, though an inter-twining of genetic, immunological, and environmental factors may play a role.
- Its manifestation varies; however, the prominent symptoms to observe include stomach pain, bloody diarrhea, cramping, weight loss, and constant fatigue.
- Prompt diagnosis and treatment could help avert conditions, such as the risk of colon tear, weight loss due to low food intake, and liver problems.
References
- Ulcerative Colitis in Children.
https://www.stanfordchildrens.org/en/topic/default?id=ulcerative-colitis-in-children-90-P02020 - Gia M Bradley and Maria Oliva-Hemker; (2012); Pediatric ulcerative colitis: current treatment approaches including the role of infliximab.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3379853/ - Pediatric Ulcerative Colitis.
https://www.yalemedicine.org/conditions/pediatric-ulcerative-colitis - Karen A Diefenbach and Christopher K Breuer; (2006): Pediatric inflammatory bowel disease.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4087963/ - Ulcerative Colitis.
https://www.chop.edu/conditions-diseases/ulcerative-colitis - Ulcerative Colitis in Children.
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02020 - Pediatric Ulcerative Colitis.
https://childrensnational.org/visit/conditions-and-treatments/stomach-digestion-gi/ulcerative-colitis-in-children - Hasan M Isa et al.; (2017); Pediatric Ulcerative Colitis from Prevalence to Outcome.
https://clinmedjournals.org/articles/jcgt/journal-of-clinical-gastroenterology-and-treatment-jcgt-3-046.php?jid=jcgt - Samy A. Azer and Yan Sun; (2022); Colitis.
https://www.ncbi.nlm.nih.gov/books/NBK541037/ - Ulcerative Colitis.
https://www.cedars-sinai.org/health-library/diseases-and-conditions/u/ulcerative-colitis.html

Community Experiences
Join the conversation and become a part of our vibrant community! Share your stories, experiences, and insights to connect with like-minded individuals.