Ventricular Septal Defect In Babies: 6 Key Insights For Parents
Breathing and feeding issues with tiredness can be a sign of ventricular defects.
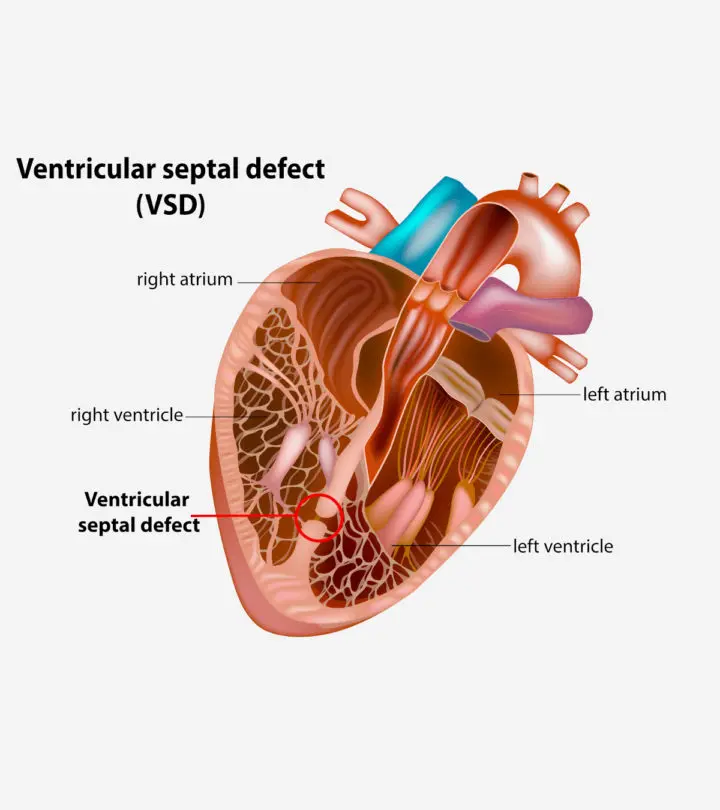
Image: ShutterStock
Ventricular septal defect or VSD in babies is the presence of an abnormal opening in the ventricular septum (the tissue or wall that separates the heart’s lower chambers known as ventricles). VSD is one of the most common congenital heart defects, accounting for nearly half of the congenital heart disease occurring in newborns.
The ventricular septum prevents the oxygenated and deoxygenated blood in the left and right ventricles, respectively, from mixing. An opening in this septum allows blood from the left ventricle to reach the right ventricle and then the lungs. Critical cases could also present reverse blood flow from the right ventricle to the left ventricle. The treatment mostly involves surgical closure of the opening, which may improve the baby’s condition.
This post explains the types, causes, symptoms, diagnosis, treatment, and prevention of VSD in babies.
Types Of VSD In Babies
Ventricular septal defects are classified into four basic types based on their location in the heart (1).
- Muscular VSD is the most common type, located in the septum’s muscular portion. This may close naturally in most babies without any surgical interventions.
- Membranous VSD is an opening in the upper part of the ventricular septum, known as a membranous septum, near the valves. This type may not close naturally and often requires surgery to close it.
- Atrioventricular canal type VSD is associated with atrioventricular canal defect. In this type, the defect is located below tricuspid and mitral valves, which are valves between the upper chambers (atria) and lower chambers (ventricles) of the heart.
- Conal septal VSD is rare and occurs below the pulmonary valve, the valve between the right ventricle and pulmonary artery leading to the lungs.
Causes And Risk Factors For VSD
VSD is a congenital heart defect, which means it is present at birth. The fetal heart development begins as a hollow tube and is later divided into four chambers. VSD could occur due to fetal heart development problems during the first eight weeks of pregnancy.
Genetic factors, such as chromosomal abnormalities, or environmental factors, such as exposure to teratogens, may interfere with the heart’s normal partition, leaving an opening in the ventricular septum (2).
Babies with a positive family history of VSD and Down’s syndrome may have an increased risk of developing VSD. In some cases, there may be no discernible cause or risk factor associated with VSD.
Signs And Symptoms Of VSD
Signs and symptoms may vary based on the size of the defect and the baby’s age. The ventricular septal defect allows blood from the left ventricle to reach the right ventricle. This may increase the work of the right ventricle and the lungs. If the hole is larger, more blood enters the heart’s right side, causing severe symptoms.
The following signs and symptoms are seen in infants with VSD (3).
- Additional blood reaching the lungs may cause congestion and rapid or heavy breathing
- Fatigue
- Sweating
- Refusal to feed
- Pale skin
- Rapid heart rate
- Poor weight gain
These symptoms and signs may also be seen in more severe congenital heart diseases. You may consult the pediatrician for early diagnosis and treatment.
Complications Of VSD
Small-size VSD may not cause any complications. Mild to life-threatening complications are often seen in babies with large and medium-size defects. These complications may include (4):
- Pulmonary hypertension (high blood pressure in the lungs’ blood vessels) can be seen in VSD due to excess blood flow to the lungs.
- Heart failure may occur in some babies since the lungs have too much blood and the heart has to work harder to pump blood.
- Endocarditis is the inflammation of the heart’s inner lining (endocardium).
- Valve failures and rhythm abnormalities may occur due to abnormal blood flow in the heart.
- Eisenmenger’s syndrome occurs in babies with severe VSD with pulmonary hypertension. This is a condition in which the direction of shunting reverses, which means the blood from the right ventricle (deoxygenated blood) begins to reach the left ventricle due to pulmonary hypertension. This may cause cyanosis in babies.
Cyanosis in a baby with previous VSD symptoms may indicate Eisenmenger’s syndrome (reversal of blood flow). You may seek immediate medical care since this may increase the risk of complications, such as cerebrovascular accidents, hemoptysis (coughing up blood), and syncope (loss of consciousness).
Prevention Of VSD In Babies
Prevention may not be possible in most cases. However, the following pregnancy care may (5).
- Preconception and early prenatal care may help the mother begin a healthy lifestyle and diet before fetal heart
- Seek prescriptions before taking medications in pregnancy to prevent fetal damage due to certain medicines.
- A balanced diet with recommended vitamins (including folic acid) and iron supplements helps the fetus’ optimal growth.
- Regular exercise during pregnancy may also be beneficial for the fetus.
- Complete vaccination status of the mother may reduce the risk of congenital defects due to infections.
- Maternal diabetic control during pregnancy may reduce the risk of heart problems in babies.
- Avoid illegal drugs, alcohol, and tobacco products during pregnancy.
If you or your partner has a family history of VSD or other genetic defects, seek genetic counseling, especially before conception.
Diagnosis Of VSD
Signs and symptoms are often suggestive of VSD in some babies. Doctors may hear heart murmurs using a stethoscope during the physical examination of babies with VSD.
The following tests are often done to diagnose the presence, size, location, and complications of the VSD in babies (6).
- An echocardiogram helps determine the size, severity, and location of the VSD and other heart problems. A fetal echocardiogram may allow diagnosis before birth.
- Chest X-ray may help to look for the heart’s size (cardiac enlargement) and excess fluid in the lungs.
- Electrocardiogram or ECG may help identify rhythm abnormalities by recording the heart’s electrical activity.
- Pulse oximetry could determine the blood’s oxygen levels. Shunting of blood may reduce the blood’s oxygen levels.
- Cardiac catheterization by inserting a catheter (thin, flexible tube) through the blood vessels of either the arm or groin could help assess the heart’s structure and function.
Babies with genetic abnormalities may require genetic testing to identify the abnormality. Doctors may plan the interventions based on the diagnostic results.
Treatment Of VSD In Babies
Small-size defects may not need surgical repair in most cases. Doctors may observe for symptoms and wait for the opening to close independently. However, small openings near the heart valves require surgical closure to prevent complications.
Medium and large VSDs may require surgical repair within the first year of life if the child has severe symptoms or is showing signs of heart failure. Treatment for VSD may include the following interventions (7).
- Medications, such as diuretics (furosemide), are often prescribed to reduce the blood circulation in the lungs.
- Extra nutrition is prescribed for babies who are tired during feeding or unable to feed themselves due to VSD to meet optimal growth.
- The catheter procedure uses a special mesh device to close the opening without a chest incision.
- Open heart surgery is done to close the opening with stitches or patches. General anesthesia is needed for this procedure, and babies are supported with a heart-lung machine.
The type of procedure is chosen based on the size of the opening and the baby’s health status. You may talk with the pediatric cardiac surgeon or cardiologist to know the best treatment option for your baby. Your baby may require several follow-up visits after the surgery to ensure improvement. Long-term prognosis may depend on the type of VSD and its severity, and adequate lifestyle management may help improve the outcome in the long run.
VSD in babies can be a major cause of concern for parents. However, it can be treated with the right type of medical assistance. To ensure that the treatment is effective, you should begin at the earliest. Don’t ignore the early symptoms of VSD, such as fatigue, sweating, and refusing to feed. Know that late diagnosis could lead to multiple complications, including heart failure. Thus, you must consult a healthcare professional to prevent any further complications at the earliest possible.
Key Pointers
- Ventricular septal defect (VSD) is categorized into four different types.
- The condition causes mixing of deoxygenated and oxygenated blood and may require surgical correction.
- Infants with VSD may show heavy breathing, fatigue, refusal to feed, rapid heart rate, etc.
- Based on severity, complications such as pulmonary hypertension, rhythm abnormalities, or endocarditis may occur.
Frequently Asked Questions
1. What is the life expectancy for a baby with VSD?
If babies have small VSD, the defect usually closes by the age of two. In some children, it may also close by the age of four. After the closure of the defect, children lead a healthy life with no restrictions.
If babies have moderate to severe VSD, they may need surgery to close the defect. After surgery, they can recover within a few weeks. You may ask your doctor how to take care of your children after surgery. Most children can lead healthy lives after recovery (3).
2. How early can VSD be detected?
VSD may be detected as early as 12 weeks of gestational age. However, in many cases, the condition is not detected until after birth (8).
References
2. Congenital Heart Defects (CHDs); The Centers for Disease Control and Prevention
3. Ventricular Septal Defect (VSD); Lucile Packard Children’s Hospital Stanford
4. Ventricular Septal Defect; MedlinePlus; U.S. National Library of Medicine
5. Ventricular Septal Defect (VSD); St. Clair Hospital
6. Ventricular Septal Defect (VSD); Children’s Hospital of Philadelphia
7. Ventricular Septal Defect (VSD); C.S Mott Children’s Hospital; Michigan Medicine
8. Ventricular Septal Defect; University of Maryland Medical Center
Read full bio of Dr. Neema Shrestha














