Zika Virus In Pregnancy: Symptoms, Risks & Prevention Guide
This mosquito-borne disease might lead to complications for the fetus if not treated soon.

Image: iStock
Zika virus spreads through the bite of an infected Aedes mosquito. However, an infected mother can pass it to the fetus, leading to complications, usually in the first trimester (1) (2). Thus, preventing exposure to the zika virus when pregnant is essential.
Generally, the zika virus exhibits mild or no symptoms, making its diagnosis difficult (3). Thankfully, vaccines can impart immunity against the virus and avert complications (4).
Read this post to learn about the zika virus infection and its symptoms, treatment, and prevention measures for pregnant women.
What Are The Signs And Symptoms Of Zika Virus During Pregnancy?
The virus has an incubation period of 3–14 days, and the disease lasts almost a week. During this time, the following symptoms may be observed (5):
- Low-grade fever
- Rash
- Joint pain
- Conjunctivitis
- Headache
- Muscle pain
Many who contract the virus are asymptomatic or develop mild symptoms that resemble other mosquito-borne illnesses such as chikungunya or dengue. But there are some exceptional cases of severe complications such as Guillain Barré syndrome, acute polyradiculoneuritis, and myelitis.
How Does Zika Virus Spread?
Zika virus spreads in the following ways (6):
- The bite of an infected Aedes aegypti mosquito
- Sexual contact
- From a pregnant woman to the fetus (placental transmission or during birth)
- Blood transfusion (7)
How Can You Prevent Zika Virus Infection During Pregnancy?
The best way to avoid Zika infection is not to travel to Zika-affected areas. If you have recently been to such places, contact your medical advisor before conception. If you live in endemic zone or your travel is mandatory, the following methods would help prevent a Zika virus infection (4) (8) (9):
- Wear light-colored clothes covering the entire body to prevent mosquito bites.
- Aedes mosquitoes attack in the mornings and early evenings; hence, try to stay indoors at such times.
- Cover the windows and doors with screens or blinds.
- Use EPA-registered insect repellents containing DEET, IR3535, or picaridin.
- If your sexual partner has traveled to an area experiencing a virus outbreak, avoid sexual intercourse for at least three to six months.
- Always use a condom during sex.
- Ensure no stagnant water is collected around the house as they are mosquito-breeding sites.
How Is Zika Virus Diagnosed During Pregnancy?
The initial diagnosis of Zika virus could be made based on the symptoms. But since the infection could be asymptomatic, blood and urine tests offer reliable diagnostics. An RT-PCR test can identify the virus’s genetic material in the blood and determine the viral load in the first seven days after the onset of symptoms. Hence, visit the doctor when symptoms begin or if you’ve recently traveled to a Zika-affected area (10) (11).
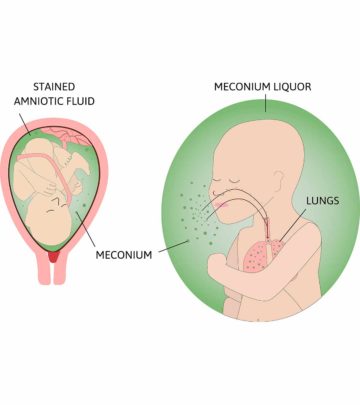
In case of Zika virus infection during pregnancy, your doctor may recommend an amniocentesis to detect the presence of the virus in the amniotic fluid (12).
Is There Any Treatment?
Unfortunately, there is no treatment for the virus. Medication is given only to treat the symptoms (fever by paracetamol). NSAIDs need to be avoided.
What Happens If You Are Infected By Zika Virus During Pregnancy?
Zika virus transmission during pregnancy could result in congenital malformations or developmental delays. Although not every child infected with congenital Zika virus may have complications, infection increases the risk of birth defects. These complications, collectively called congenital Zika syndrome, could include (13)
- Microcephaly (abnormally small head) in infants
- Limb contractures
- Hearing loss
- High muscle tone
- Eye defects
- Brain development abnormalities
- Seizures
- Psychomotor developmental delays during childhood
Fetuses who contract the Zika virus in utero may not show health problems in the beginning. Since these complications may manifest later in life, they must be screened soon after birth. The following tests may be conducted in their first month (14):
- Physical examination
- Blood, urine, and cerebrospinal fluid analysis
- Ultrasound of the brain
- Eye examination
- Auditory brainstem response (ABR) to check the brain’s response to auditory cues
The medical provider will determine if any abnormal results are due to the Zika virus and provide healthcare based on the complication.
How Long After A Zika Virus Infection Is Pregnancy Safe?
If you have been to an area with a Zika virus outbreak, the waiting period is two months after travel or the onset of symptoms. However, this period is longer for men since the virus may be found in their semen for nearly three months after travel or Zika infection. During this time, sexual intercourse is not advised to prevent sexual transmission (15).
Frequently Asked Questions
1. Does the Zika virus affect pregnancy in the third trimester?
Yes. Although the risk for congenital abnormalities is more with exposure to the Zika virus in the first trimester, they may also occur from the contraction of the virus in the second or third trimester (16).
2. Do Zika babies survive?
According to a cohort study, babies born with congenital Zika syndrome may have a higher mortality rate than those born without it (17). Moreover, if the Zika virus affects babies’ brains, causing a condition called smooth brain, they may have either a low survival rate beyond two years or have no concerning health issues (18).
3. Can Zika be detected in a fetus?
Yes, fetal ultrasound may help detect Zika virus-induced brain abnormalities of the fetus during the second and third trimester (19).
4. Does the Zika virus affect future pregnancies?
No, according to the CDC, it is unlikely that a previous Zika virus exposure can affect future pregnancies since they will be protected from future Zika infections (20).
Despite large Zika virus outbreaks in the US in 2015 and 2016, firm preventive measures have reduced its impact since 2019. Nevertheless, care must be taken by pregnant women if they or their partners have visited Zika-affected areas. In such cases, early visits to a doctor for diagnosis are recommended.
Key Pointers
- A Zika virus infection could cause a low-grade fever, joint pain, or headache.
- It usually spreads through mosquito bites and sometimes through blood transfusion or unprotected sexual intercourse.
- A Zika virus infection during pregnancy may alter fetal development and increase the risk of congenital disabilities such as microcephaly and brain development anomalies.
- If you’ve recently visited a Zika virus-affected area, undergoing diagnostic tests could help prevent the spread of the infection.
References
- About Zika.
https://www.cdc.gov/zika/about/index.html - Data and Statistics on Zika and Pregnancy.
https://www.cdc.gov/pregnancy/zika/data/index.html - What Is Zika Virus?
https://www.hopkinsmedicine.org/zika-virus/what-is-zika-virus.html - Zika Virus.
https://www.who.int/news-room/fact-sheets/detail/zika-virus - Symptoms: Zika Virus.
https://www.cdc.gov/zika/symptoms/symptoms.html - Prevention And Transmission.
https://www.cdc.gov/zika/prevention/index.html - Zika and Blood Transfusion.
https://www.cdc.gov/zika/transmission/blood-transfusion.html - Protect Yourself & Others.
https://www.cdc.gov/zika/prevention/protect-yourself-and-others.html - Protecting Yourself and Your Family from the Zika Virus.
https://www.hhs.gov/zika/protect/index.html - Algorithm For Zika Virus Diagnosis.
https://main.mohfw.gov.in/sites/default/files/73633636501455013085_1.pdf - Information about Zika virus testing.
https://www1.health.gov.au/internet/main/publishing.nsf/Content/ohp-zika-testing.htm - Zika Virus And Pregnancy.
https://www.marchofdimes.org/complications/zika-virus-and-pregnancy.aspx - Birth Defects.
https://www.cdc.gov/zika/healtheffects/birth_defects.html - Care For Babies Affected By Zika.
https://www.cdc.gov/pregnancy/zika/family/care-for-babies-with-congenital-zika.html - Questions About Zika.
https://www.cdc.gov/zika/about/questions.html - Zika Virus.
https://mothertobaby.org/fact-sheets/zika-virus-pregnancy/ - Enny S. Paixao et al. (2025); Mortality from Congenital Zika Syndrome — Nationwide Cohort Study in Brazil.
https://www.nejm.org/doi/pdf/10.1056/NEJMoa2101195 - CONGENITAL ZIKA SYNDROME.
https://www.marchofdimes.org/complications/congenital-zika-syndrome.aspx - Zika and Pregnancy: Prenatal Care.
https://www.cdc.gov/pregnancy/zika/testing-follow-up/prenatal-care.html#:~:text=During%20pregnancy%2C%20healthcare%20providers%20canof%20congenital%20Zika%20virus%20infection. - Zika virus: Questions About Zika.
https://www.cdc.gov/zika/about/questions.html#:~:text=Once%20someone%20has%20been%20infectedbirth%20defects%20in%20future%20pregnancies.
Essential Zika Virus Prevention Tips for Pregnancy
Watch this video to learn how to spot Zika symptoms in pregnancy and apply proven prevention strategies. Stay informed on safe diagnosis methods to protect your baby. Watch now!