Here’s Why Your Blood Group Is Important In Pregnancy
Understanding how your unique antibodies and compatibility impact maternal and fetal health.
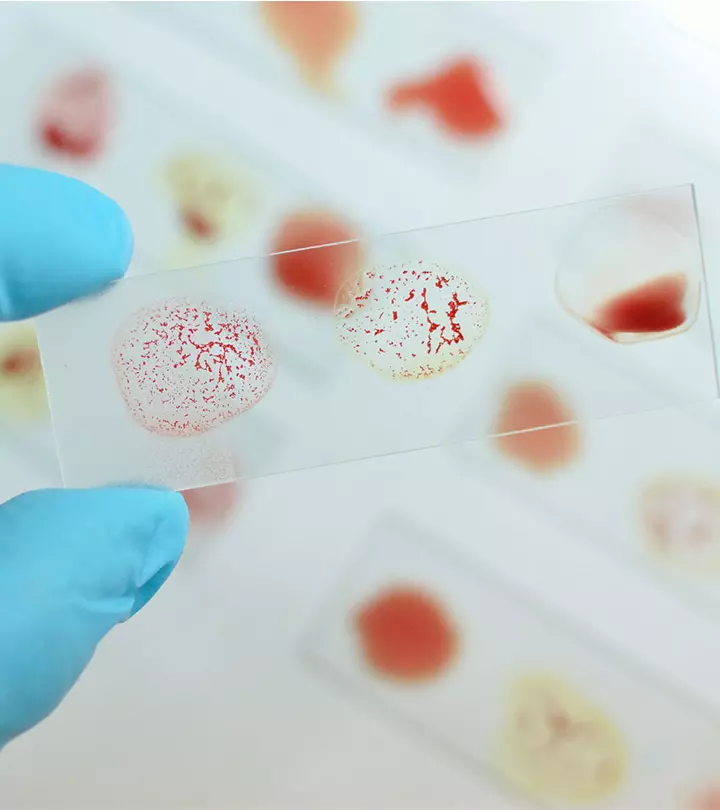
Image: iStock
Most of the times you might not care for what blood group you belong to unless you have to mention it for any paperwork. Even your ID card might ask this information of you. It is to make you aware of your blood group should you need a transfusion or should you want to donate your blood at any point in time. Once blood group could either be friendly or destructive to the other, therefore, they ascertain the blood groups before any transfusion. However being aware of blood group before pregnancy is a different ball-game. Let us explain why.
We are all aware that blood groups are classified into A, B, AB and O blood groups, each of which has a specific characteristics belonging to them alone. These blood groups carry antigens on your red blood cells and produce antibodies against other group antigens. For instance, a woman whose blood group is A carries type A antigens on her red blood cells that help identify these cells as her own. She would also carry antibodies against type B blood cells called anti-B antibodies that destroy any type B blood cells in her body.
On the other hand, a woman whose blood type is B carries B antigens on her blood cells and has anti-A antibodies that would destroy type A blood cells in her body.
Those with AB blood group have both A and B antigens and have neither of the A nor B antibodies.
Those with O blood group have no antigens on the blood cells but have anti-A and anti-B antibodies.
There are other antigens but when it comes to pregnancy, it is the D antigen that matters and here’s where you will understand the role played by the Rhesus factor.
Your blood may or may not harbor Rhesus factor. If Rhesus factor accompanies the blood type it is positive, else it is negative. For instance, if an A type blood group has Rhesus factor, it would be known as A+ or A positive blood group. Similarly we have B+, AB+, and O+ blood groups while those devoid of the Rhesus factor are negative, viz., A-, B-, AB- or O-.
A positive or a negative blood group doesn’t matter much until you are pregnant because there could be health issues for the fetus or the fetus of the next pregnancy. In fact the rhesus factor provides a protective coating around the blood groups (as in positive blood groups) while it is not so in the case of negative blood groups.
What happens when you have an Rh positive blood, and your partner has Rh negative blood group or vice versa? Your baby might have positive or negative blood group. If you are a positive and your baby is negative, it will not put your fetus at risk because your blood has the protective Rhesus fact on the blood cells that can help encounter another blood type in small doses. However, if you are a negative and your baby has a positive blood group, your body might produce antibodies against the baby’s blood in case the blood of you and your baby mix!
The greatest likelihood of the blood mixing occurs when the placenta comes away from the uterus after birth. If there is no medical intervention, the antibodies that are produced against baby’s positive blood can be a matter of concern for subsequent pregnancies as well because these antibodies will build up and a similar attack on baby’s blood cells would occur if the future pregnancy also carries a fetus with the positive group.
Here’s why a serum (anti-D or anti-D gammaglobulin) is injected to prevent the mothers from producing more antibodies that would attack the Rh-positive blood of the fetus.
The baby’s blood type won’t be confirmed until after delivery and for this reason, there are precautionary measures taken during your pregnancy to decrease the likelihood of adverse reactions. Women with negative blood groups are administered an anti-D injection at 28 weeks and 34 weeks of gestation to avert early sensitization.
Once the baby is born, its blood group is determined from the sample collected from the umbilical cord. A Kleihauer test is performed within the first 24 hours after delivery to see if the mixing of the fetal and mother’s blood has occurred and during this period the results are confirmed.
If the baby is Rhesus negative, there is no further anti-D required, else the baby is give one final dose of anti-D within 48 hours after birth, thereby, making in three shots of anti-D in all. The same procedure applies to other negative blood groups as well. In a few instances, additional anti-D is required but are restricted to miscarriage, abdominal trauma, vaginal bleeding or other invasive procedures.